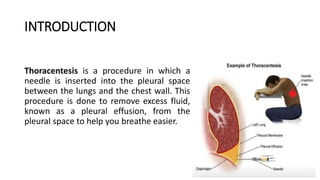
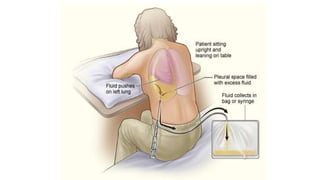
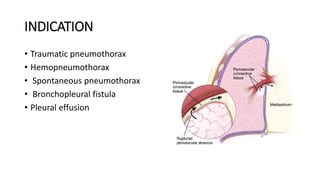
Thoracentesis is a medical procedure used to remove excess fluid from the pleural space to alleviate breathing difficulties, diagnose underlying issues, and relieve pain. Key indications include pleural effusion and pneumothorax, with contraindications that include coagulation disorders and severe respiratory conditions. Nursing responsibilities involve patient education, preparation for the procedure, and monitoring post-operation to ensure patient safety and comfort.