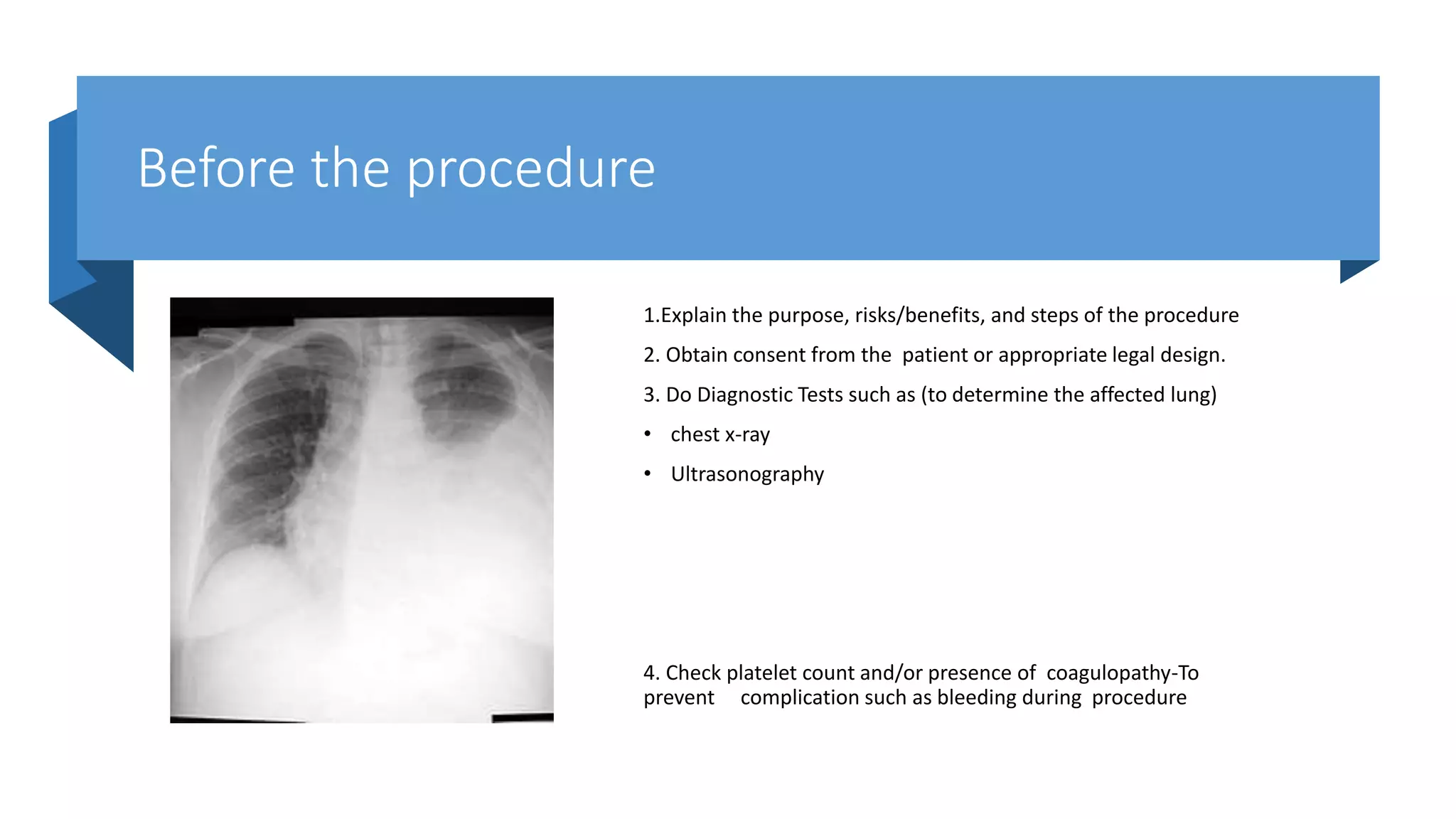
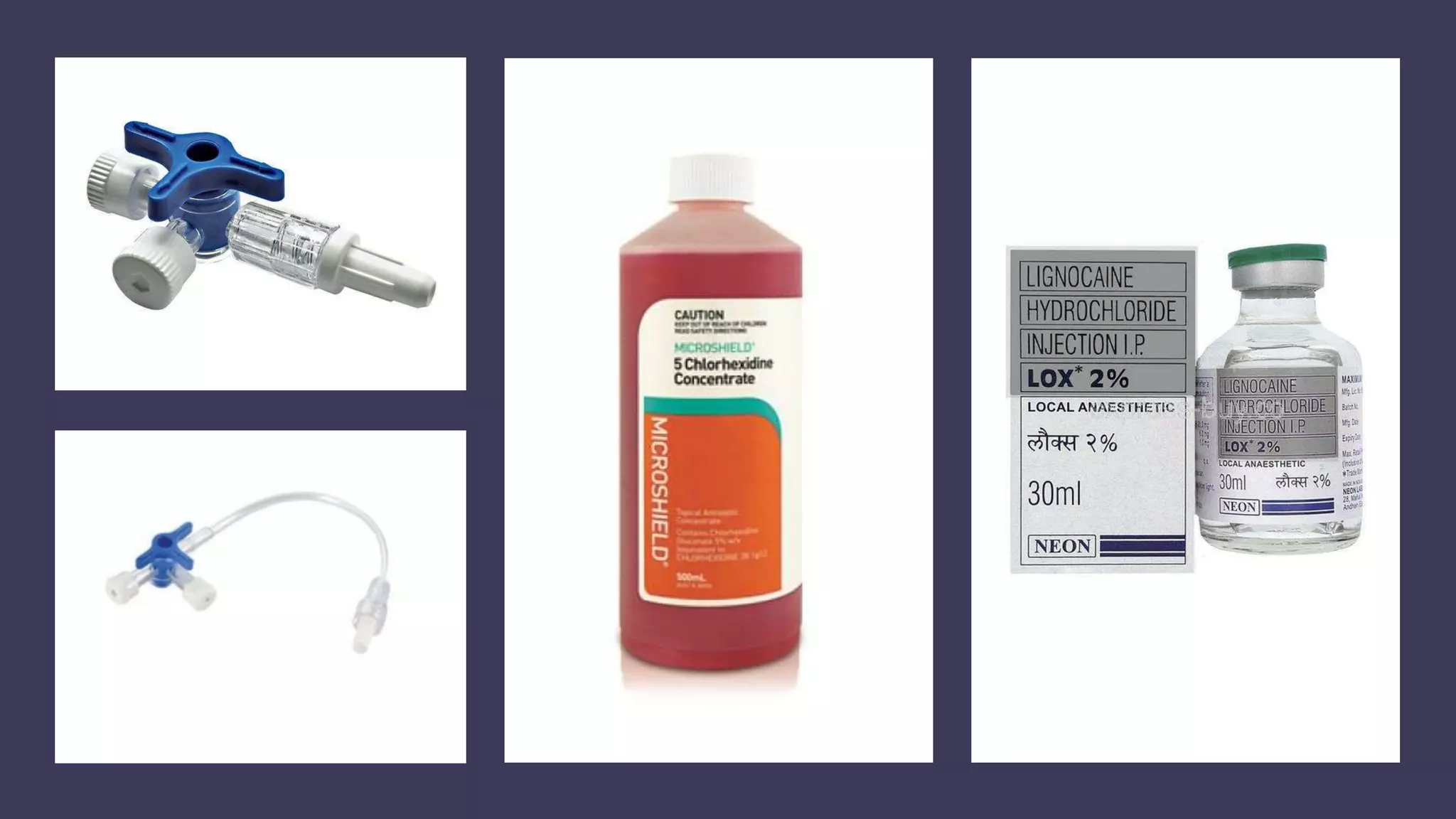
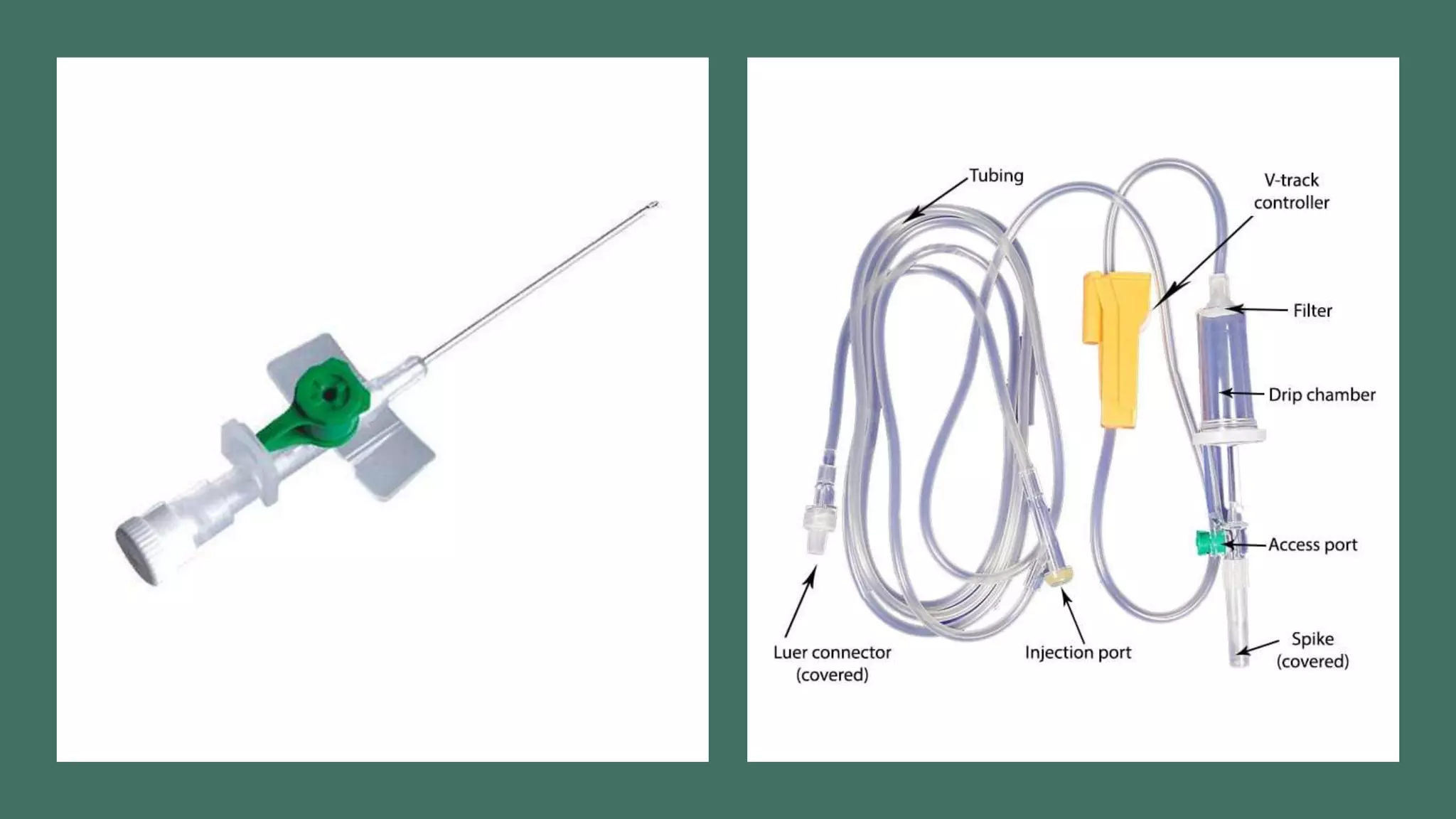
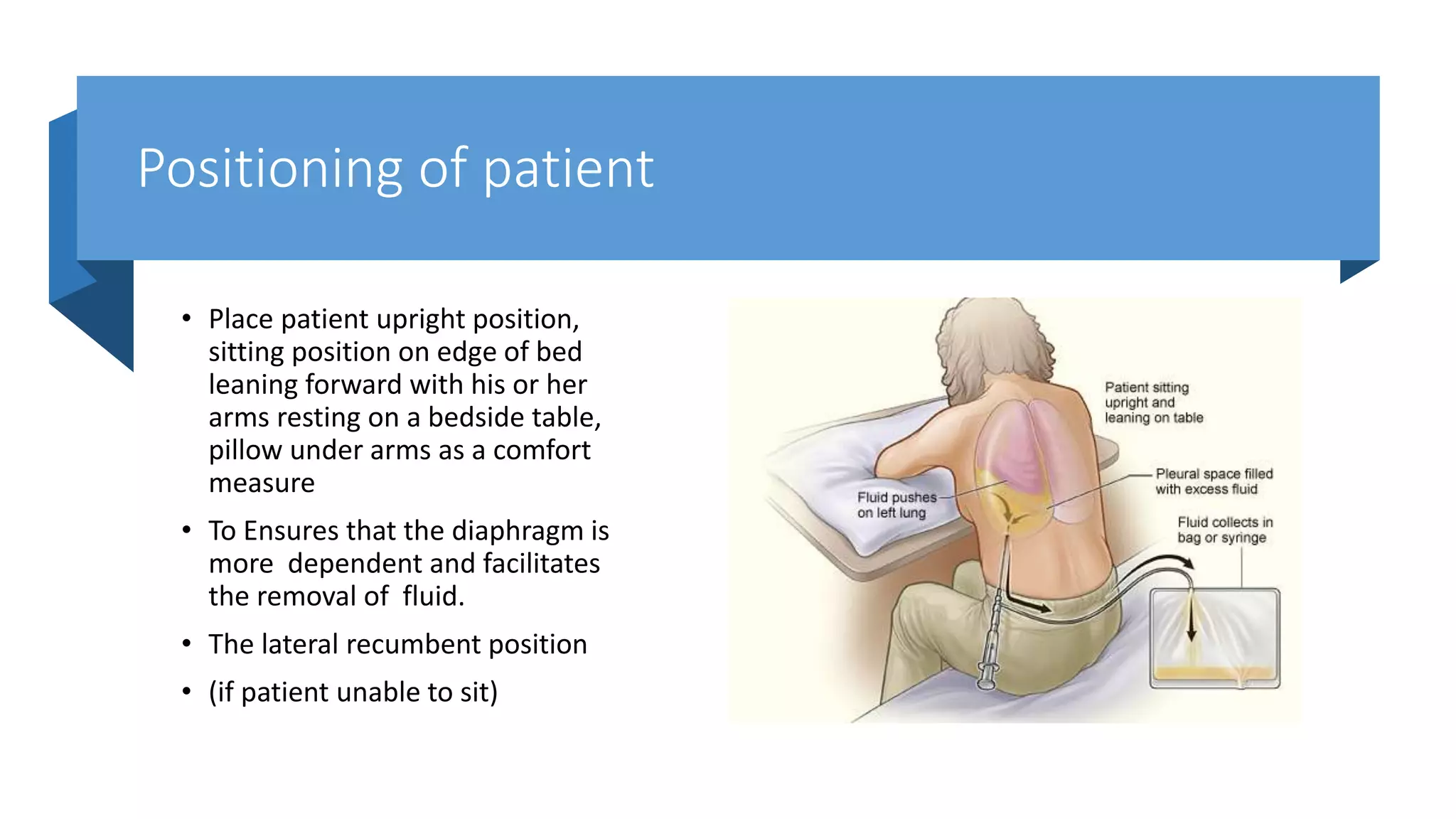
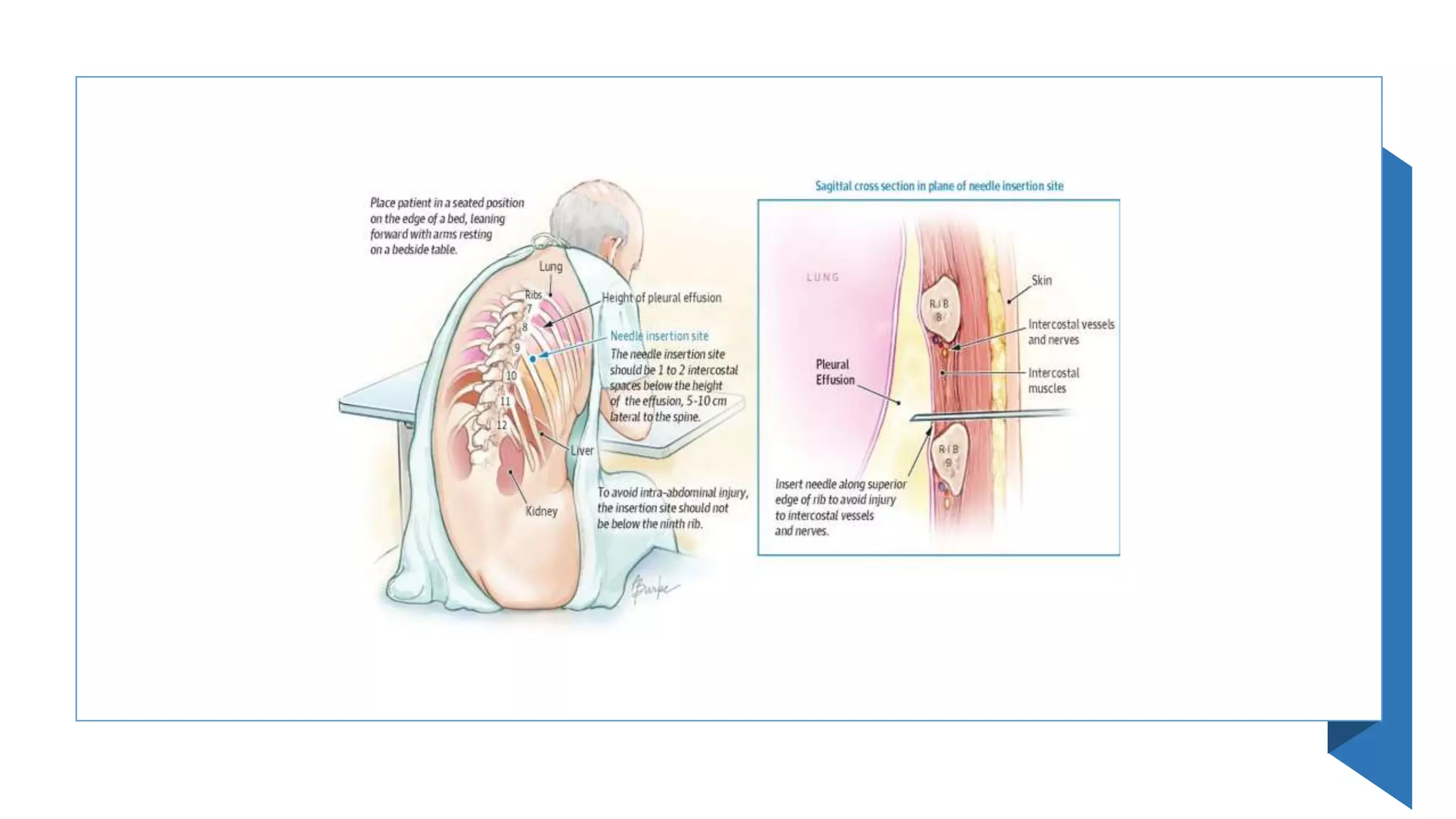
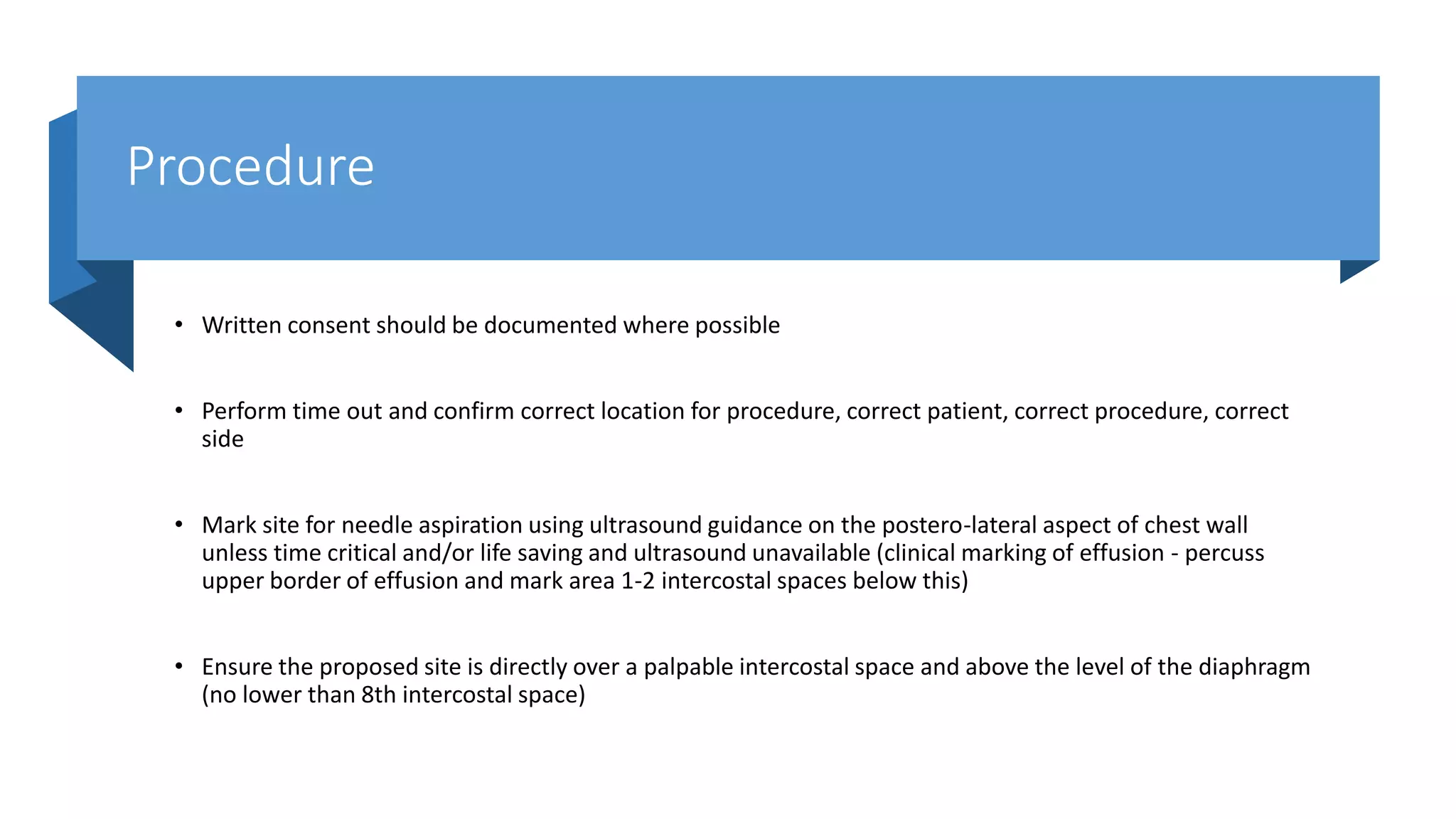
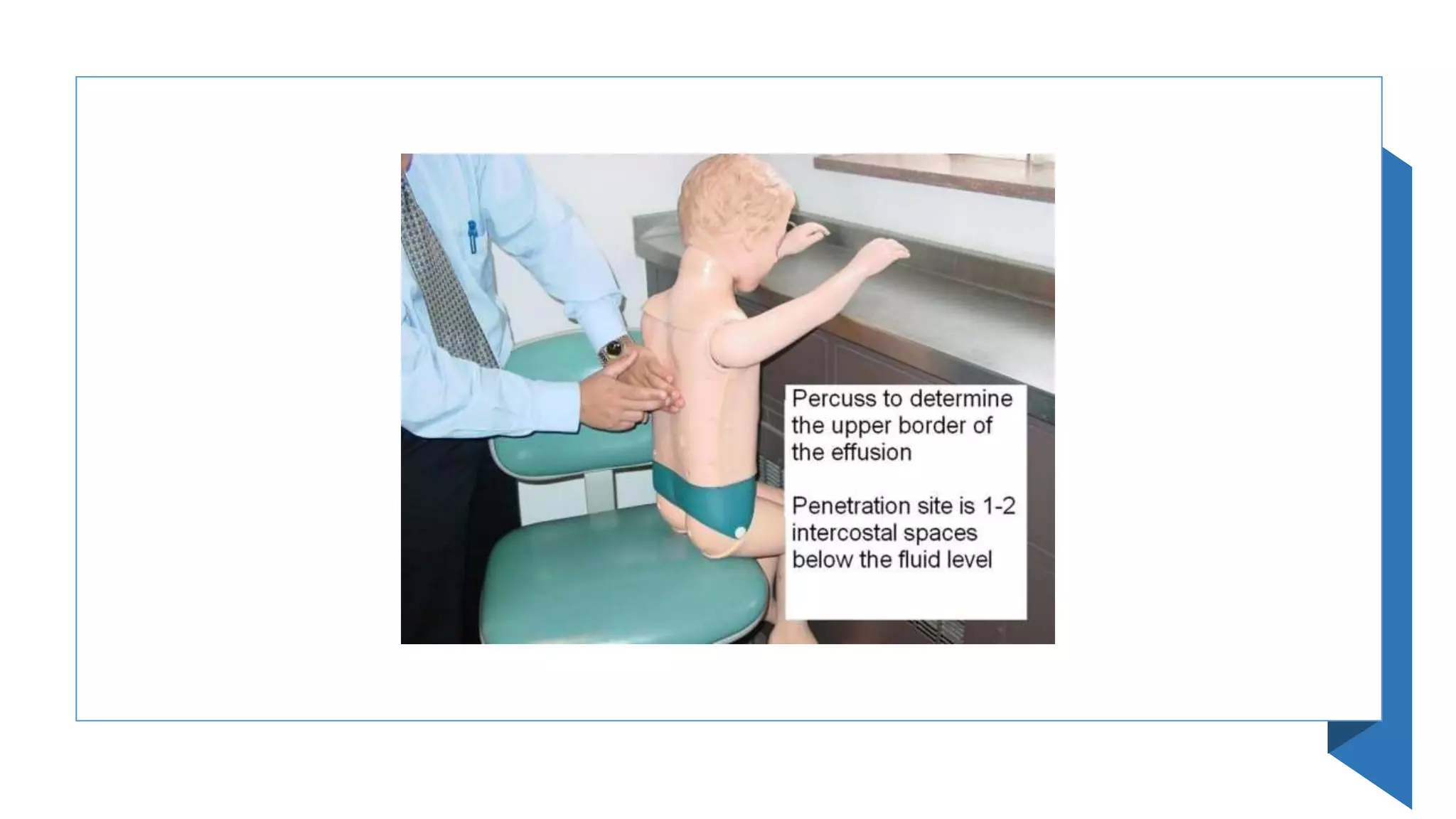
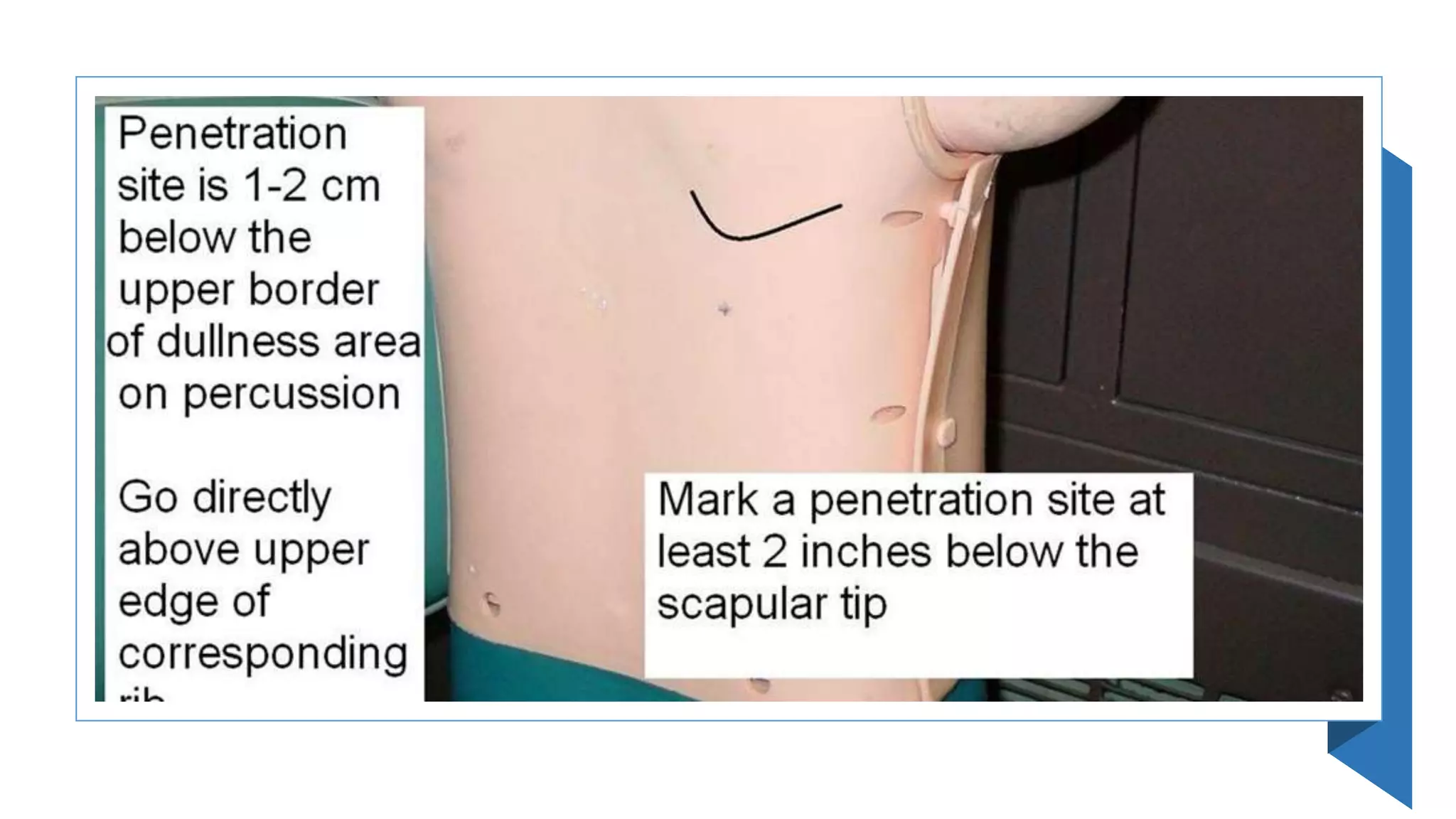
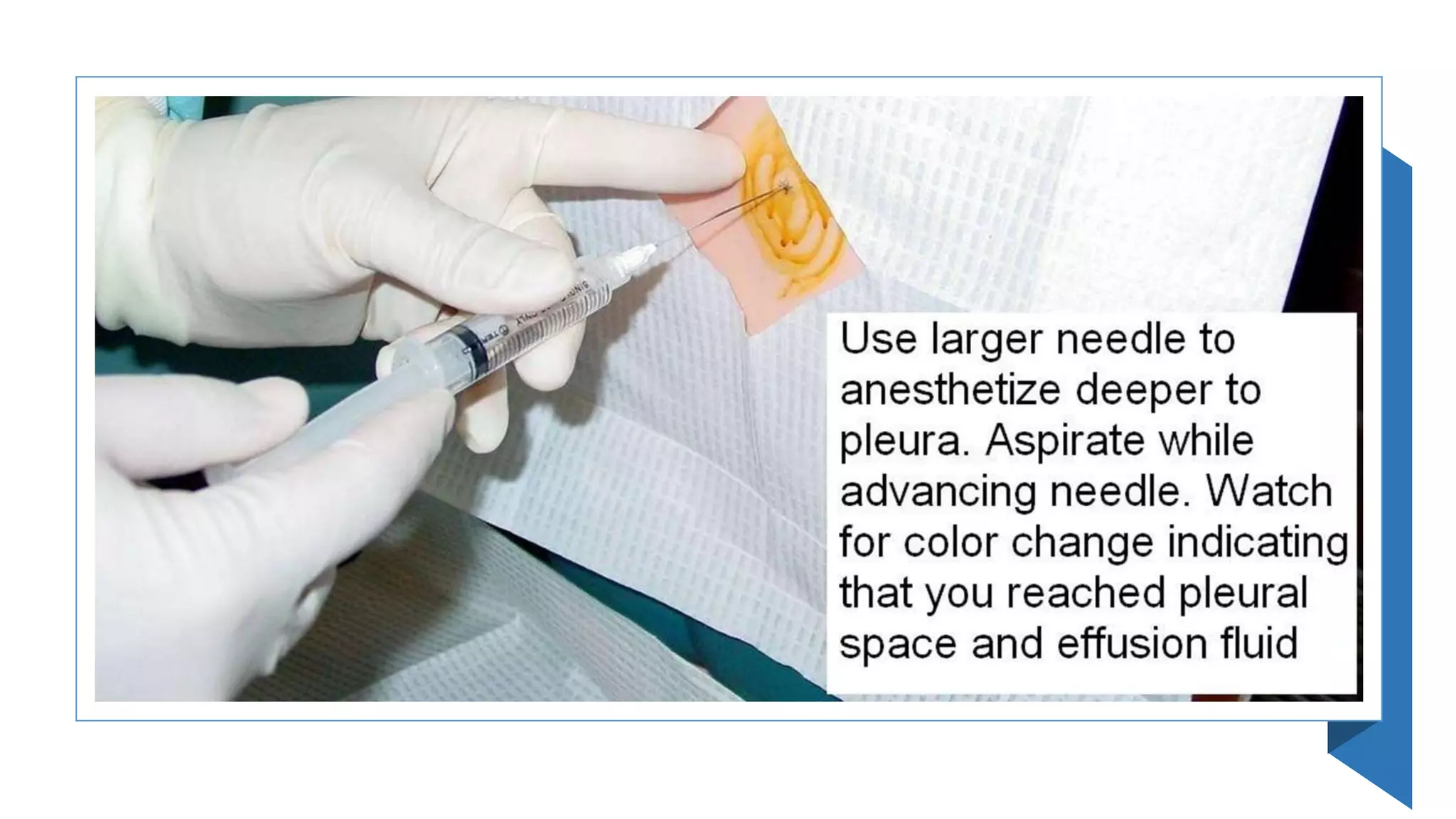
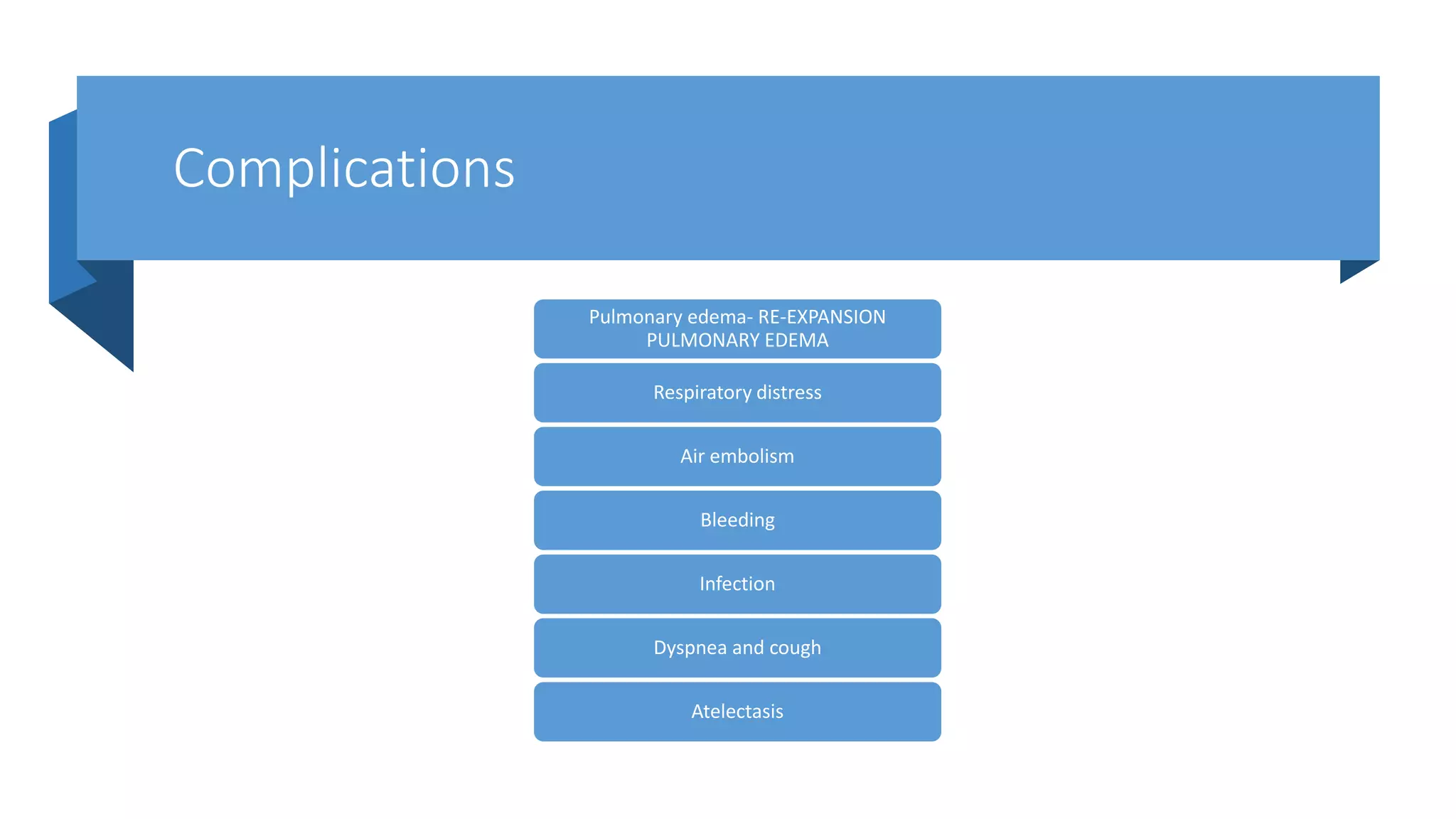
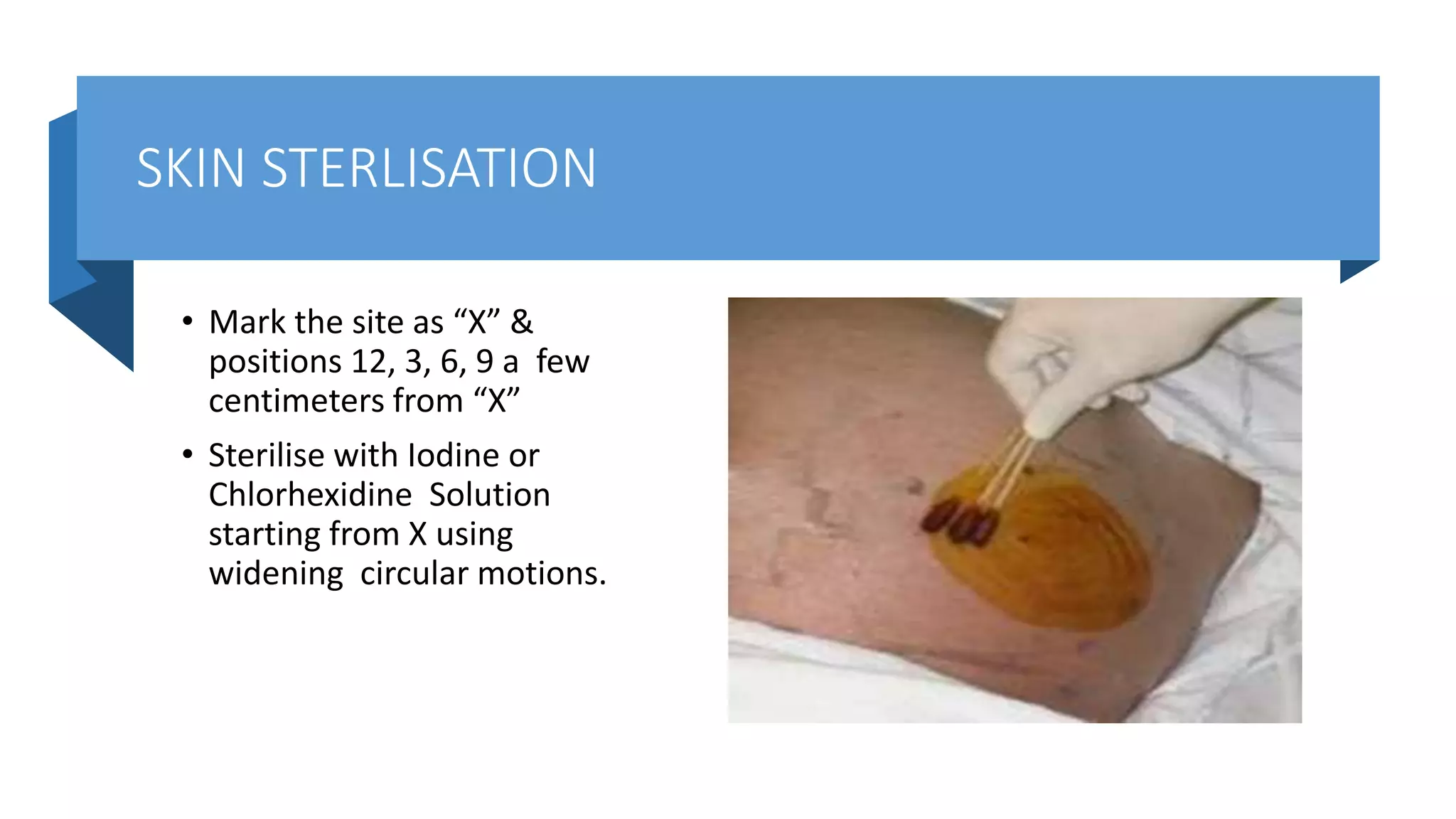
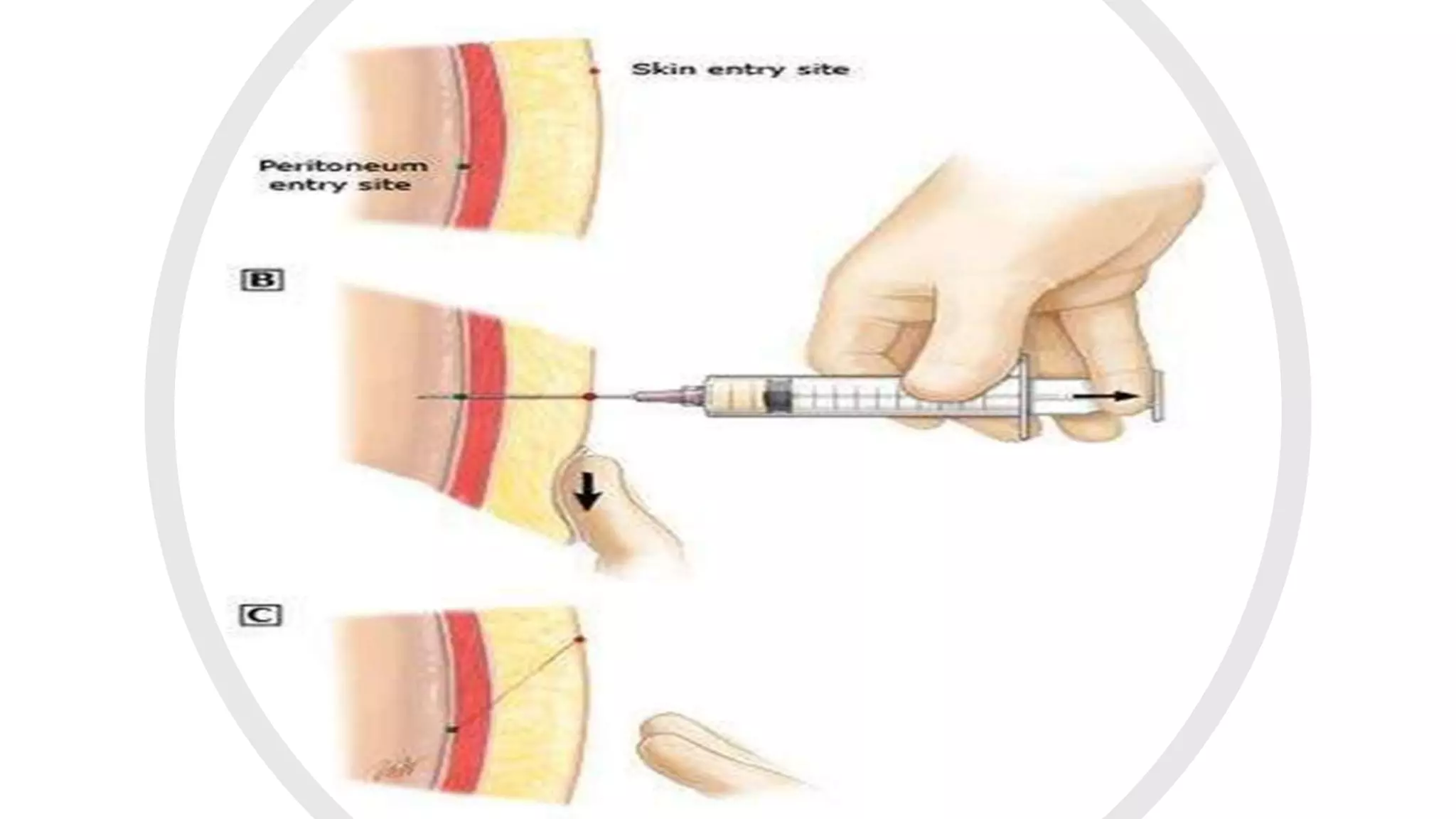
This document provides instructions for performing a thoracentesis procedure. It describes the indications, contraindications, necessary equipment, patient positioning, steps of the procedure, monitoring during the procedure, post-procedure care, potential complications, and instructions for abdominal paracentesis. The key steps are: administering local anesthesia, inserting a cannula or needle into the pleural space, draining pleural fluid for diagnostic testing or therapeutic relief of symptoms, and monitoring for complications such as pneumothorax after the procedure.