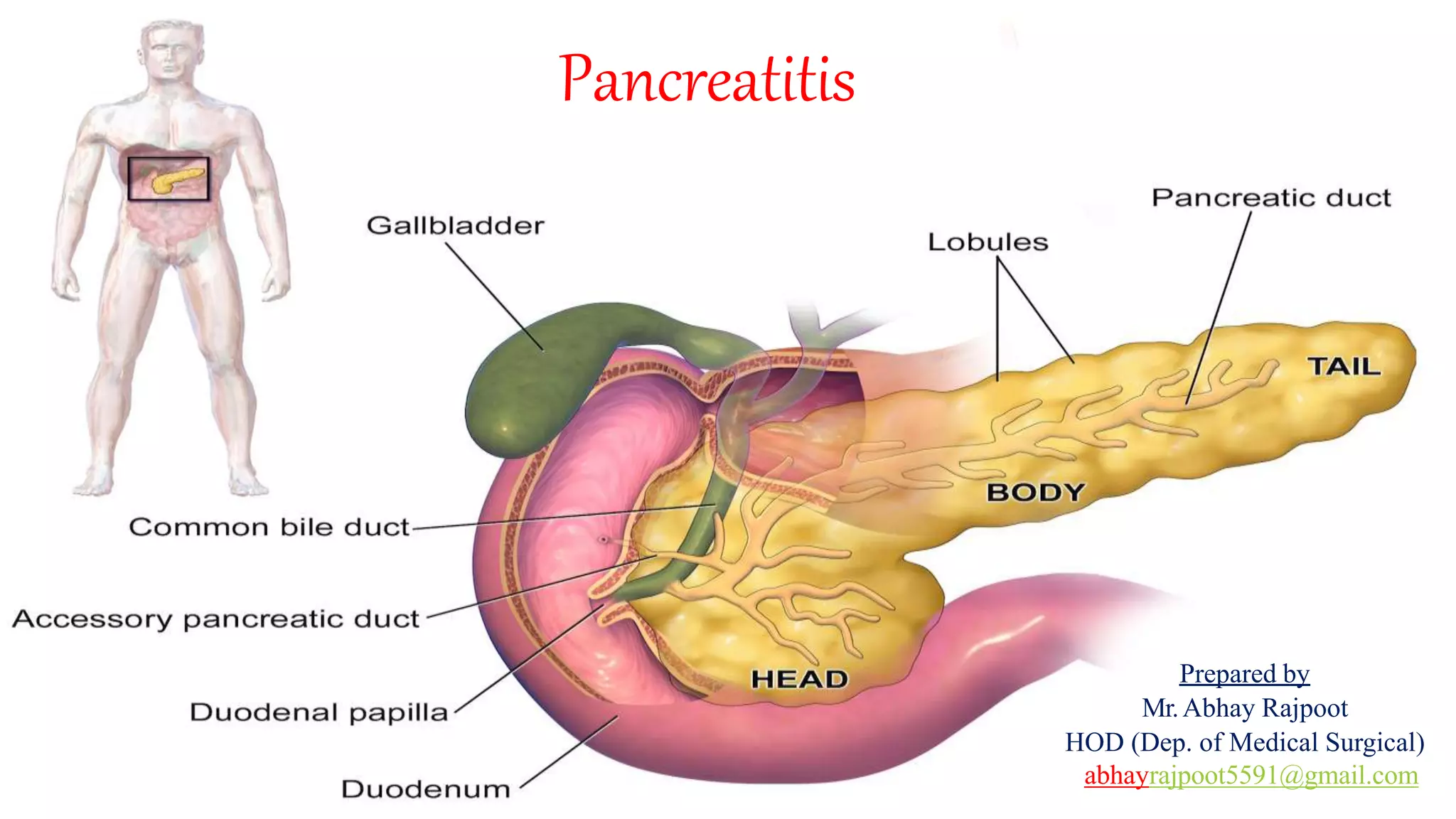
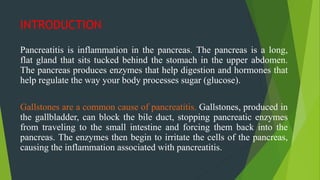
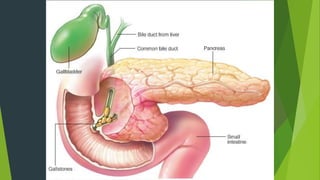
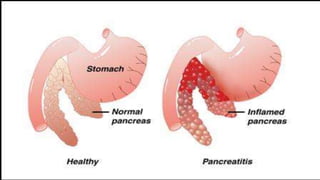
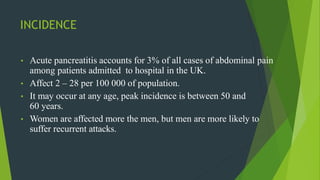
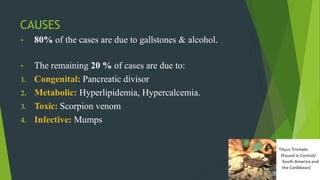
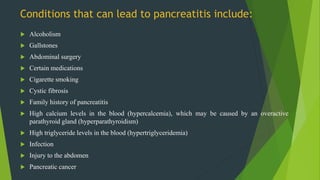
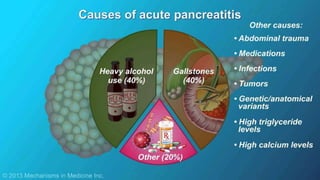
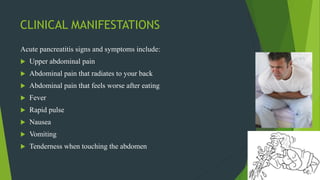
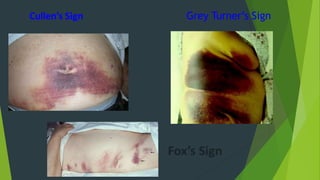
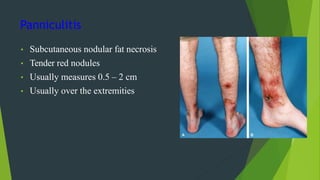
Pancreatitis is inflammation of the pancreas, which can be acute or chronic, often caused by gallstones and excessive alcohol consumption. Symptoms include abdominal pain, nausea, and fever, while risk factors may include smoking, obesity, and genetic predisposition. Diagnosis involves blood tests and imaging studies, and management may require fluid resuscitation, analgesics, and sometimes surgery to address underlying causes.