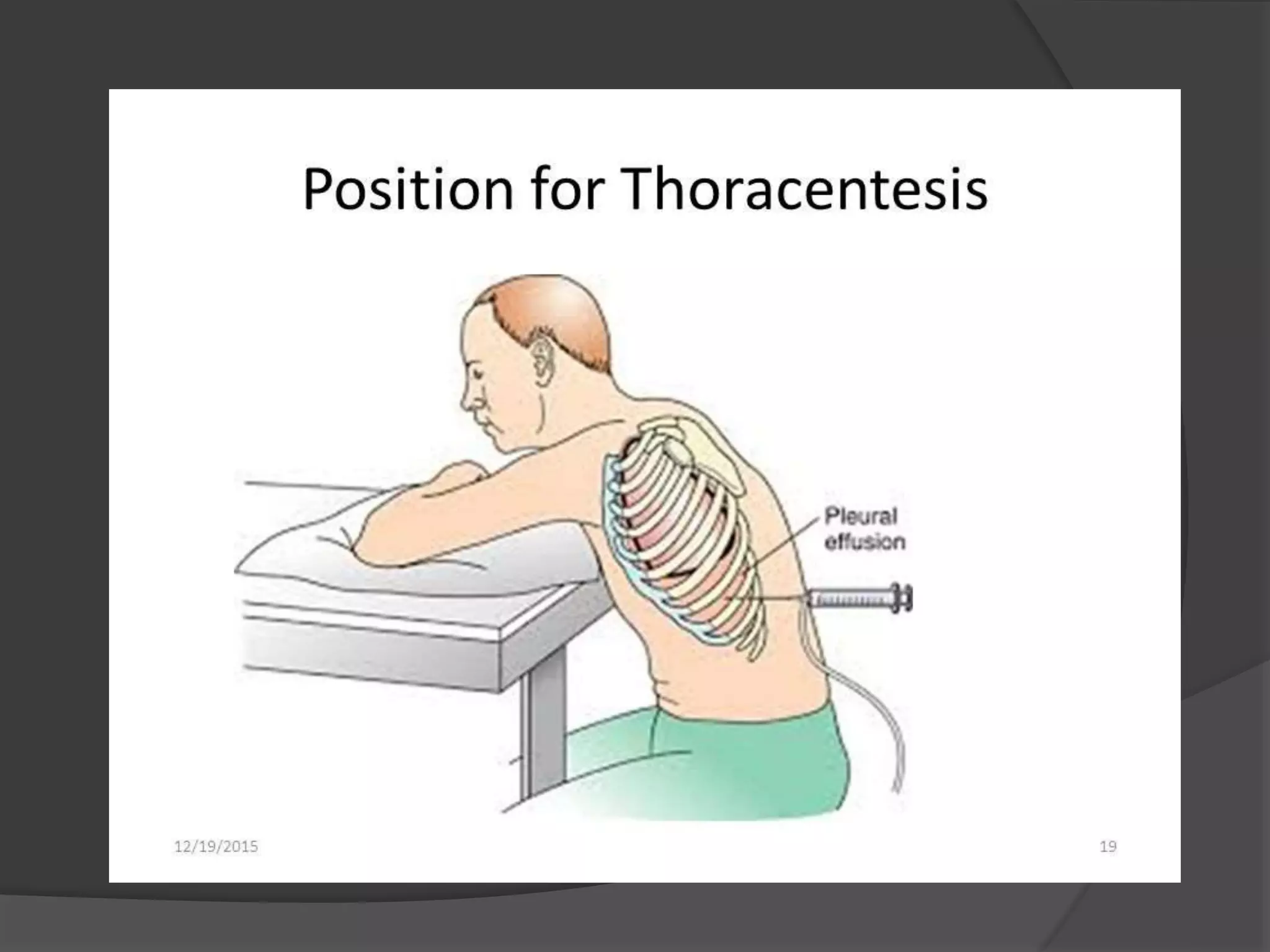
Thoracentesis is a procedure to remove fluid or air from the pleural cavity through insertion of a needle into the chest wall. It is indicated for conditions such as pleural effusion, pneumonia, or trauma. The nurse prepares equipment like syringes, needles, and specimen containers and assists the physician by administering local anesthetic, observing for complications, and providing aftercare like monitoring for bleeding or infection. Precise technique and positioning are important to safely drain fluid and avoid injuries to lungs during the procedure.