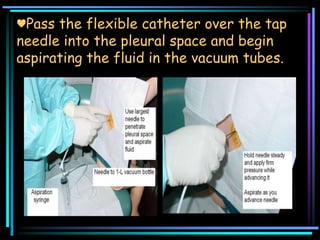
Thoracentesis is a procedure to remove fluid from the pleural space for diagnostic or therapeutic purposes. It involves inserting a needle through the chest wall after administering local anesthesia. The fluid is tested to determine the cause of the pleural effusion and guide treatment. The patient will be monitored for complications after the procedure such as difficulty breathing or signs of infection before being discharged.