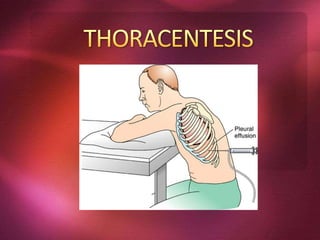
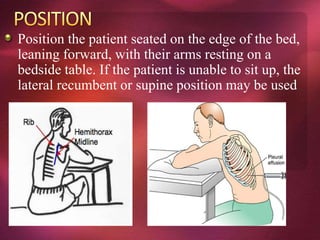
Thoracentesis is a medical procedure that involves the removal of fluid from the pleural space around the lungs to diagnose or treat conditions like pleural effusions. The procedure carries risks such as pneumothorax and requires careful management of contraindications and complications, especially in patients with respiratory issues or coagulopathy. Proper patient positioning, monitoring, and specimen analysis are crucial steps in ensuring patient safety and obtaining accurate diagnostic results.