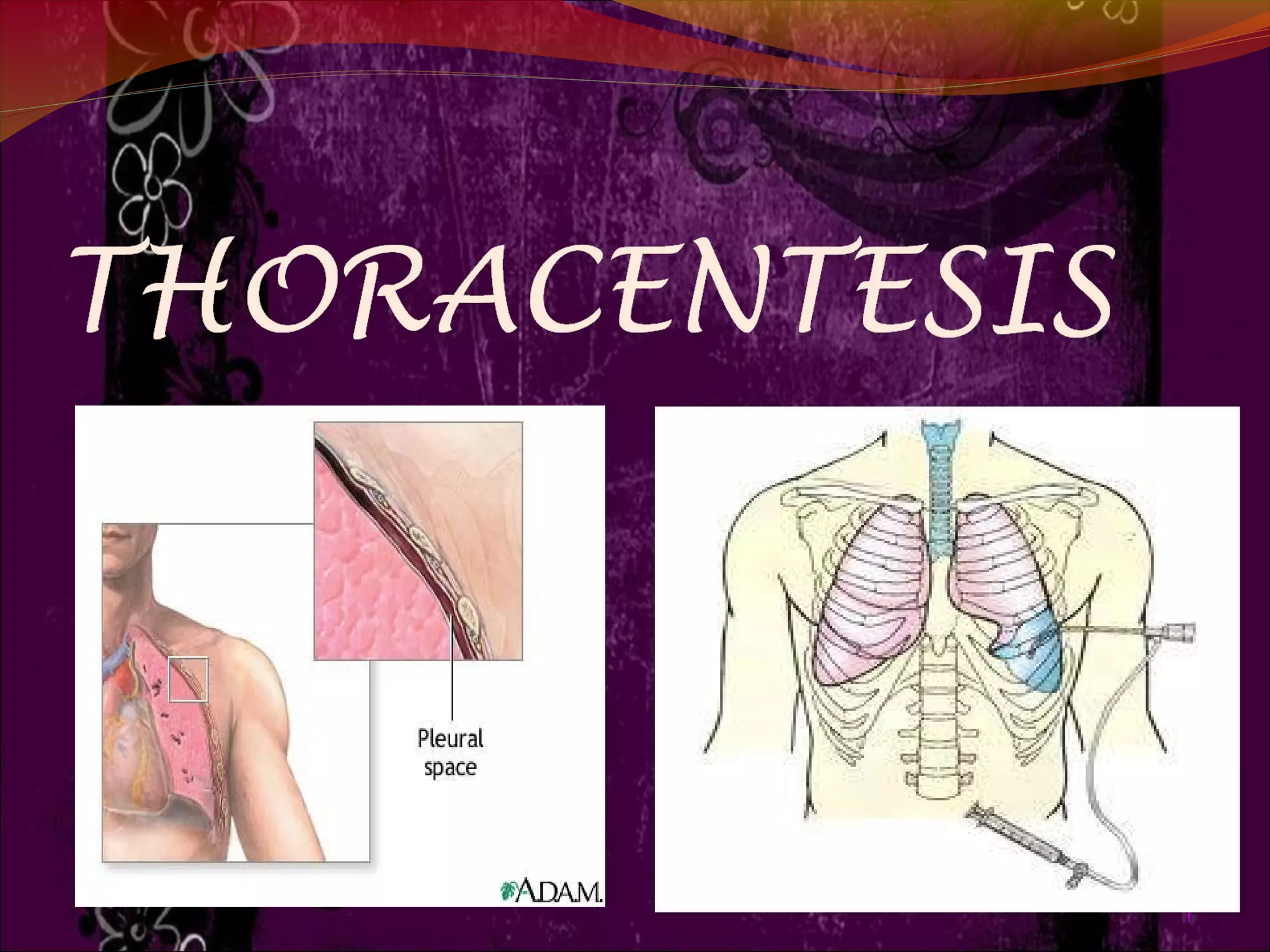
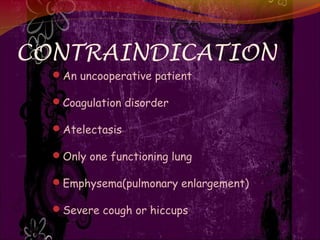
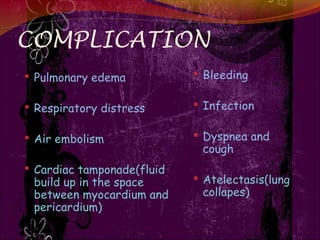
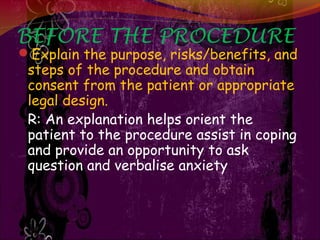
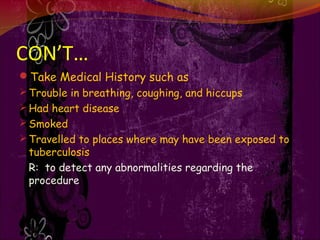
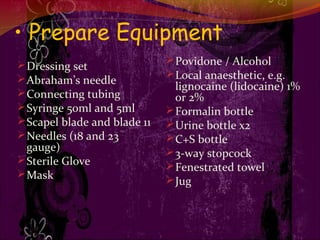
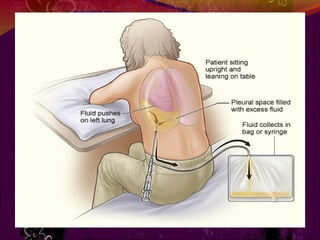
This document discusses the procedure of thoracentesis, which involves removing fluid from the pleural space between the lungs and chest wall through a needle or tube. It defines thoracentesis and provides information on its purpose, indications, contraindications, complications, pre-procedure preparation, the procedure itself, and post-procedure care. The main points are that thoracentesis is done to diagnose or treat abnormal fluid accumulation in the pleural space and relieve related symptoms. Proper preparation, monitoring during the procedure, and post-care are important to minimize risks and ensure the health and comfort of the patient.