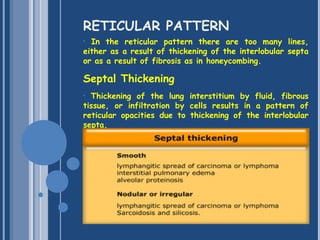
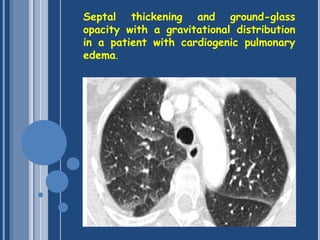
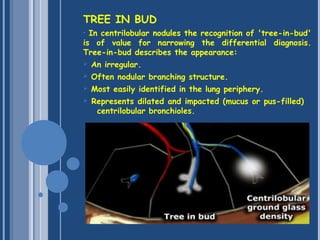
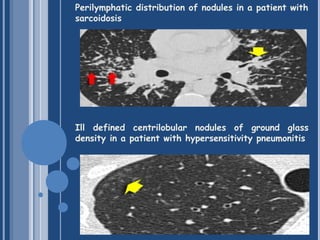
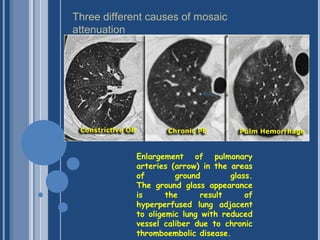
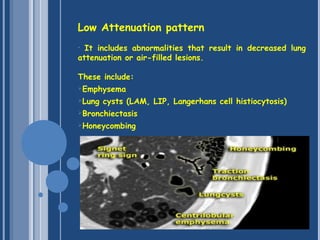
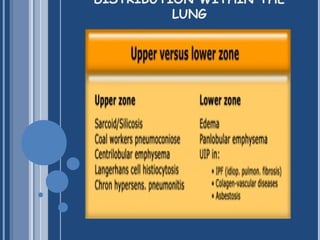
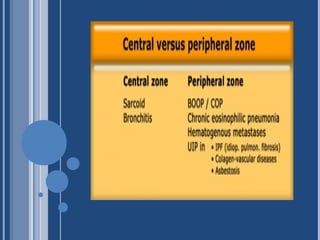
The document discusses the basic interpretation of HRCT scans of the lungs. It describes the anatomy of the secondary lobule and how diseases can affect the centrilobular or perilymphatic areas. Common patterns seen on HRCT like reticular, nodular, ground glass and consolidations are explained. The distribution of abnormalities within the lungs and specific signs like tree-in-bud are also covered.