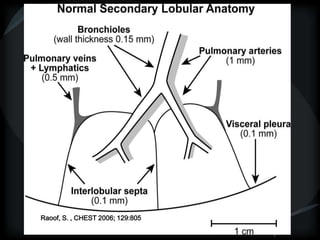
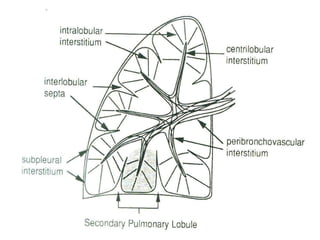
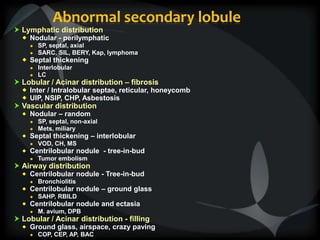
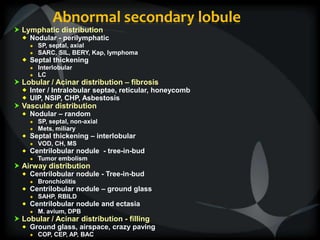
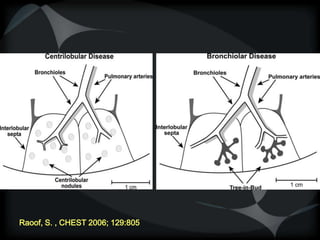
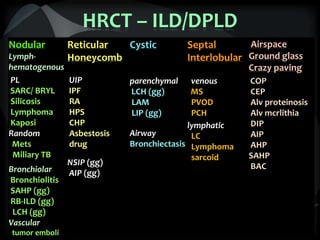
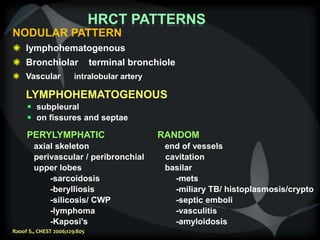
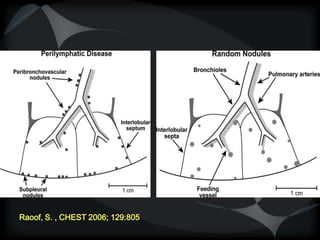
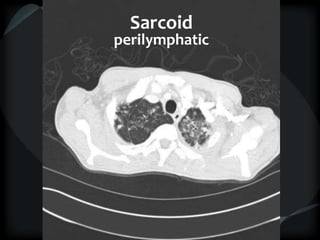
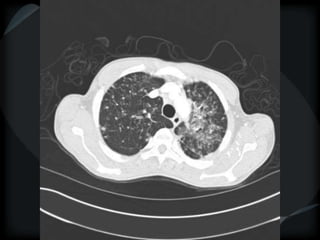
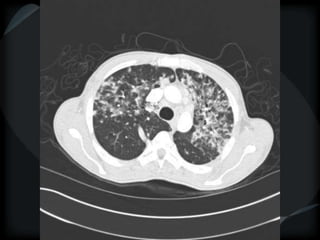
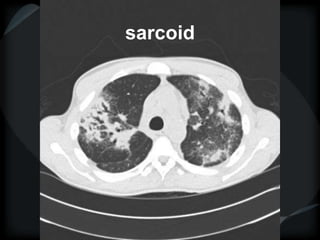
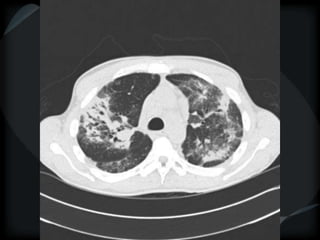
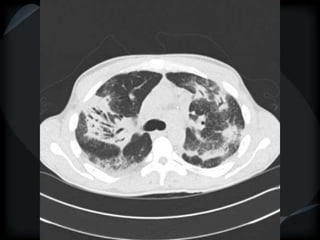
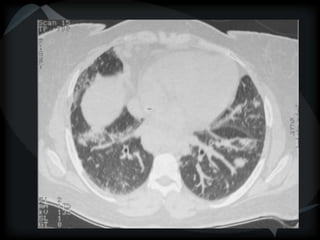
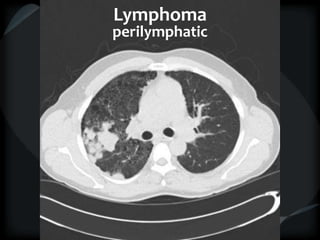
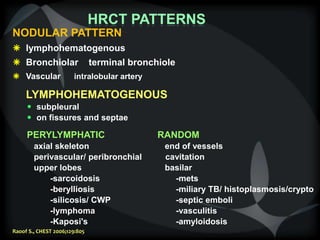
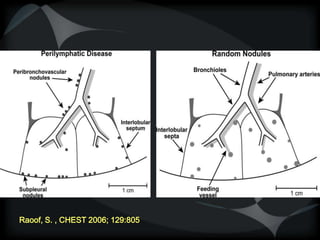
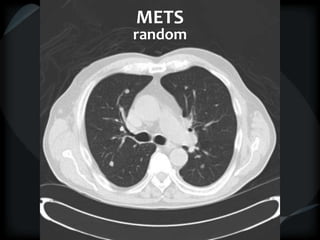
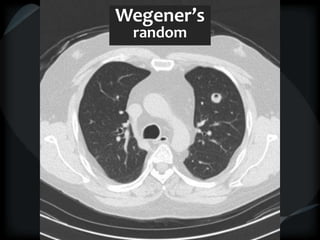
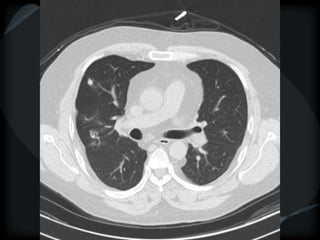
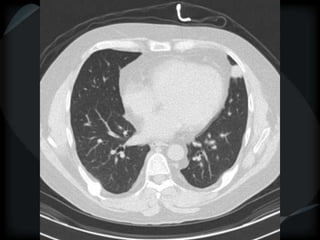
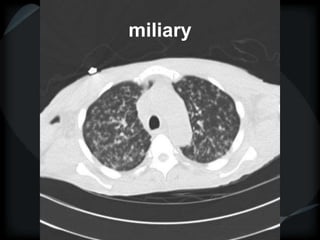
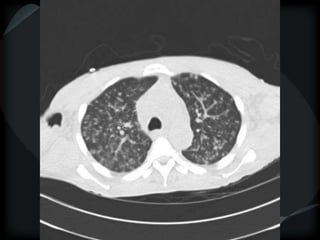
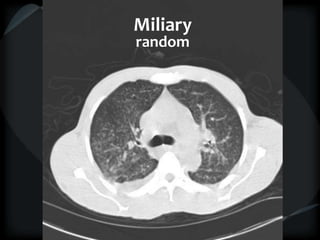
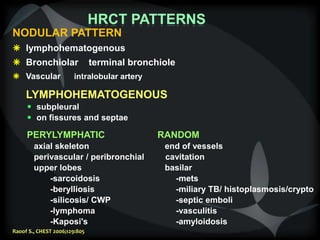
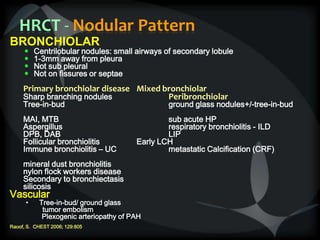
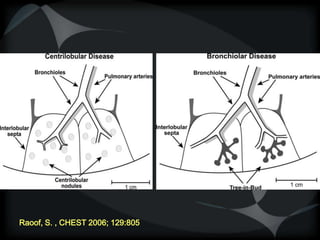
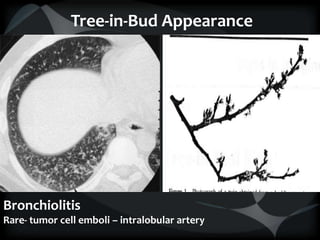
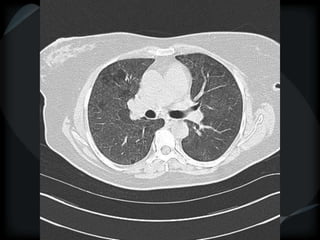
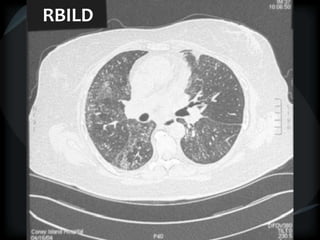
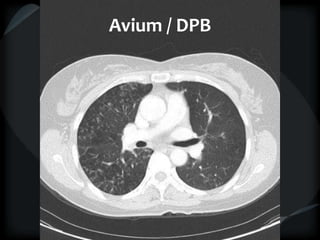
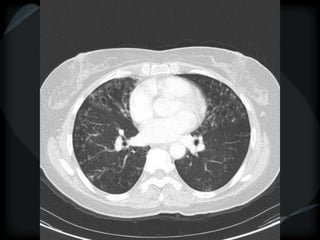
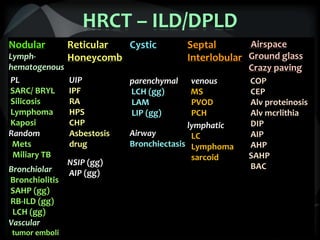
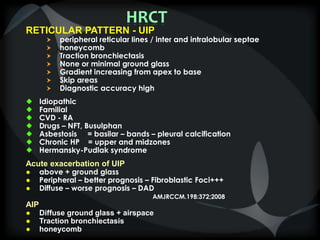
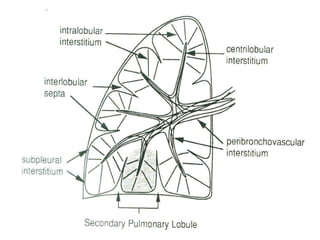
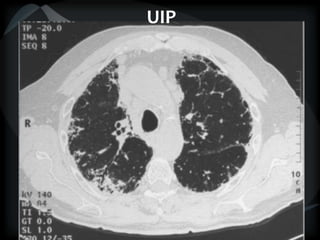
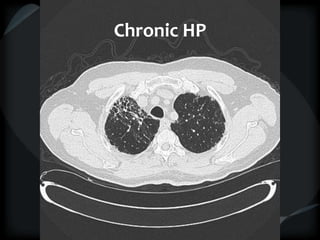
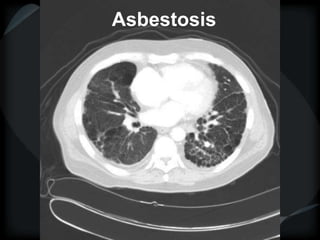
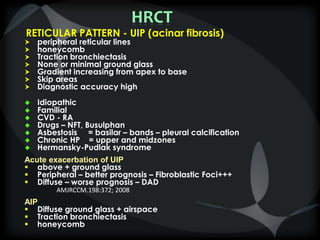
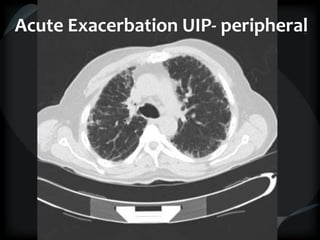
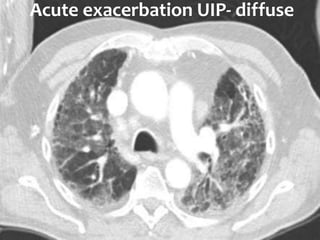
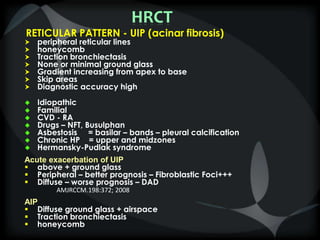
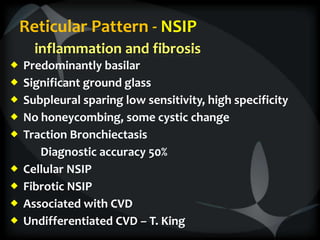
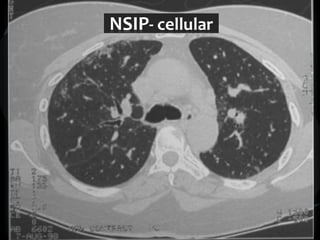
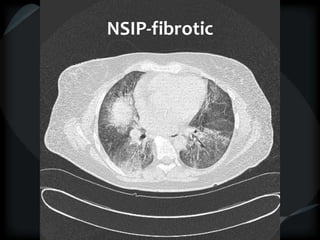
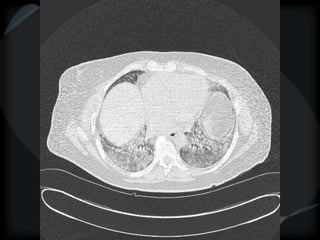
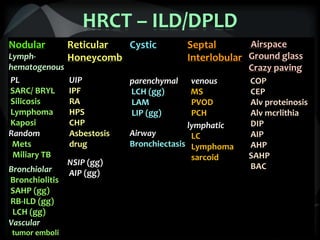
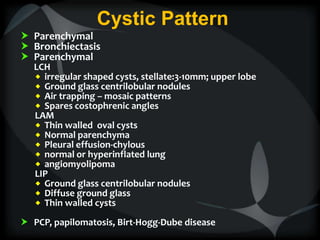
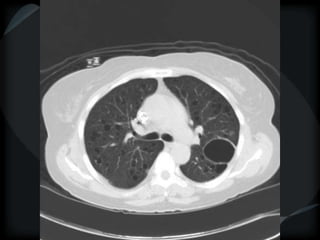
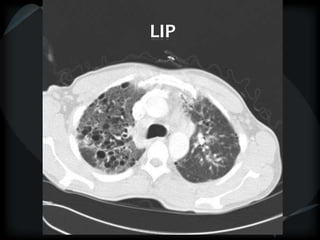
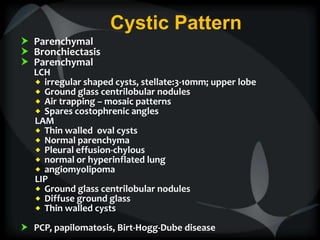
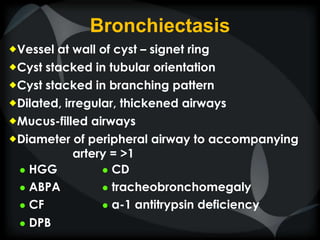
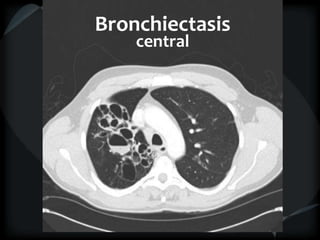
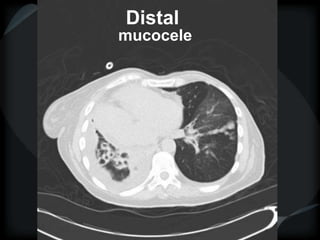
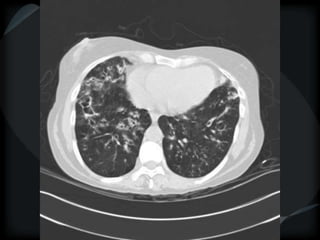
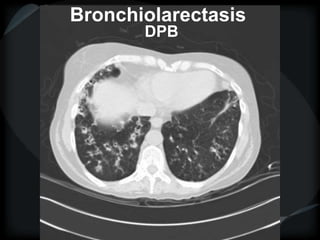
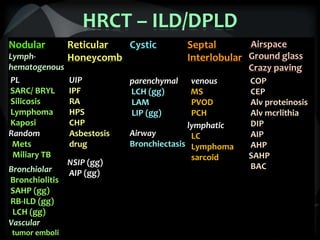
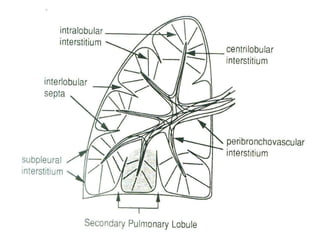
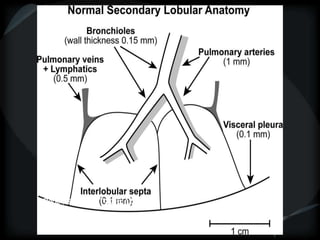
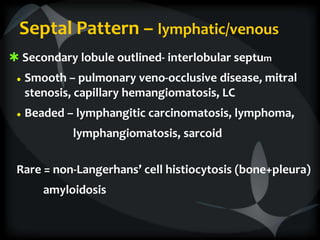
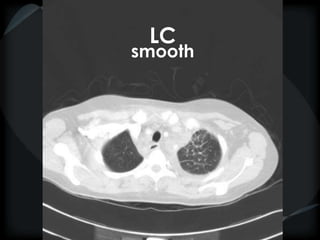
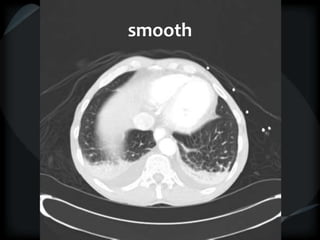
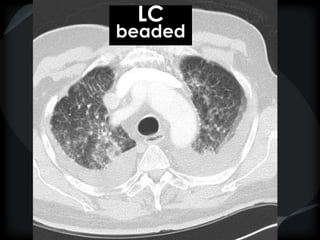
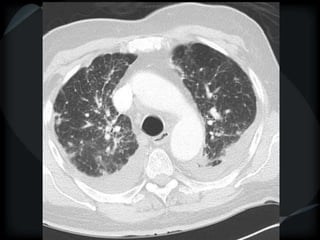
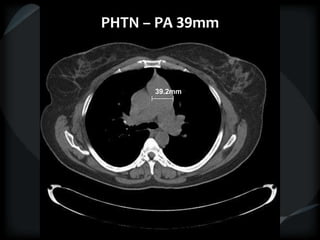
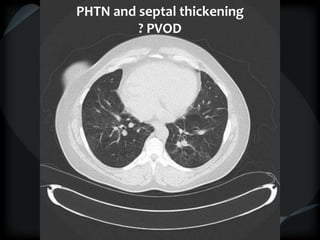
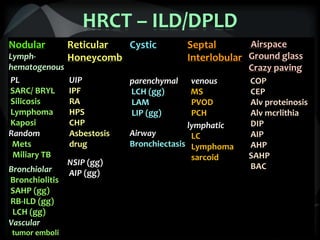
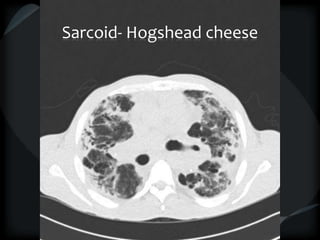
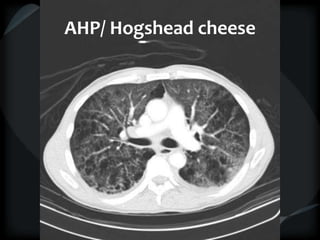
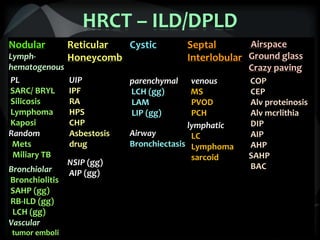
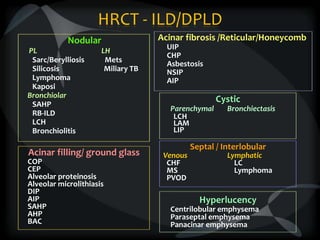
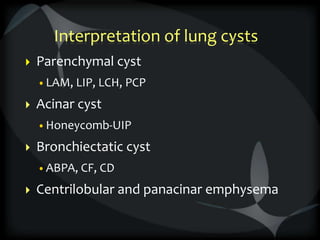
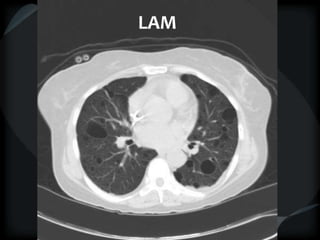
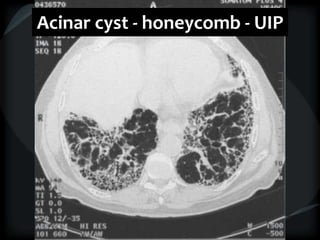
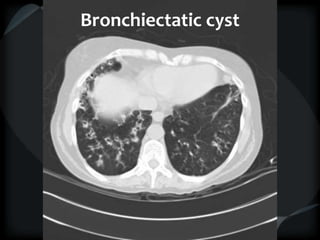
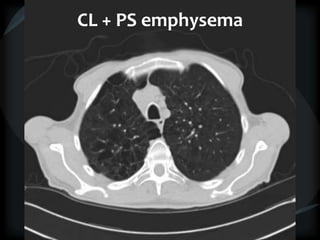
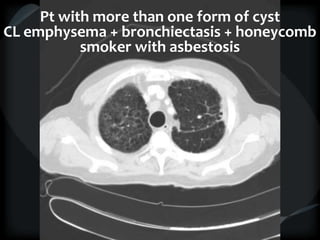
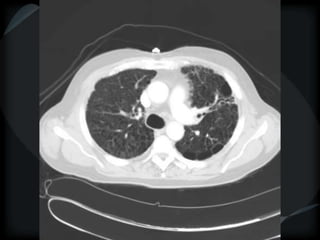
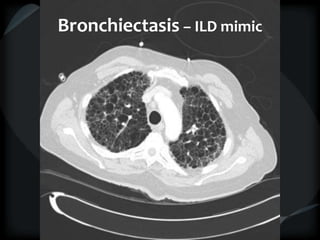
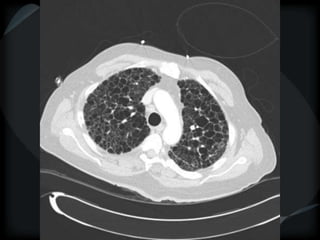
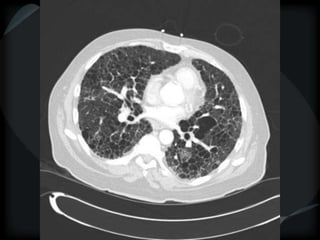
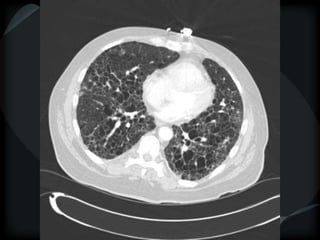
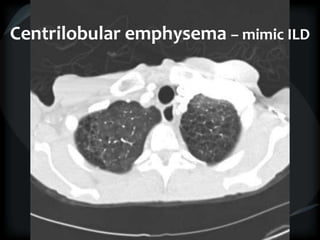
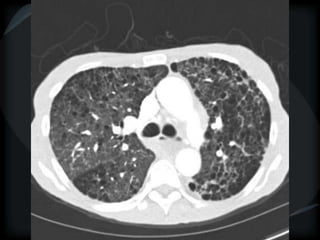
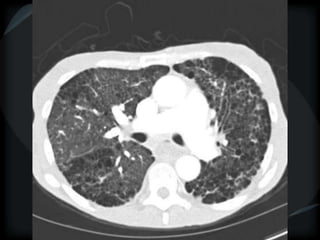
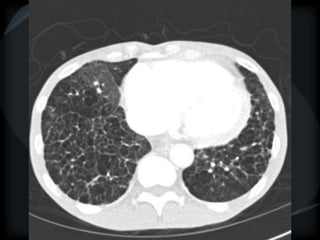
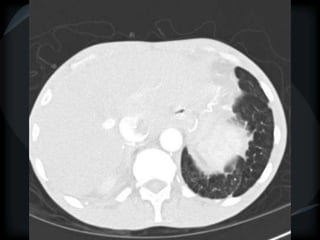
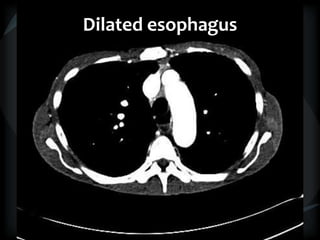
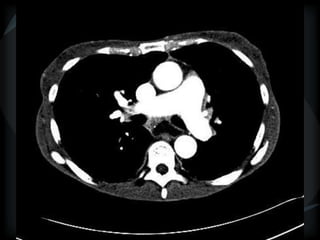
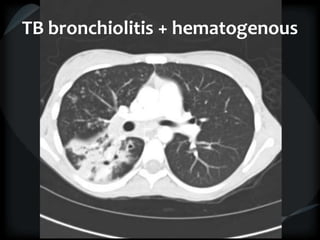
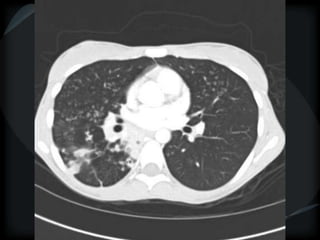
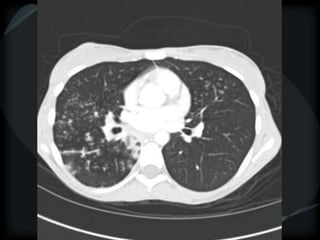
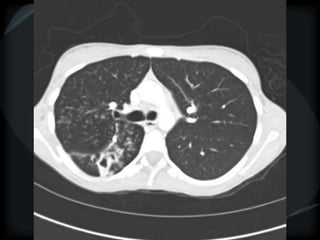
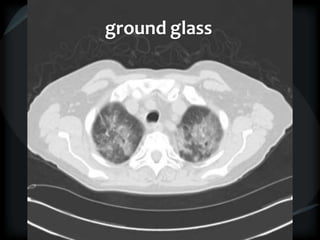
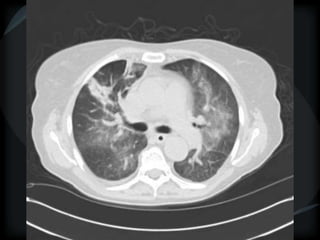
This document discusses patterns seen on HRCT that can help characterize different lung diseases. It describes the nodular, reticulation, cystic and airway patterns seen in conditions such as sarcoidosis, lymphoma, metastases, pulmonary fibrosis, bronchiectasis and others. Key findings include perilymphatic nodules in sarcoidosis, random nodules in metastases, honeycombing and reticulation in idiopathic pulmonary fibrosis, and cysts in lymphangioleiomyomatosis. Differentiating these patterns on HRCT can provide clues to diagnose underlying lung abnormalities.