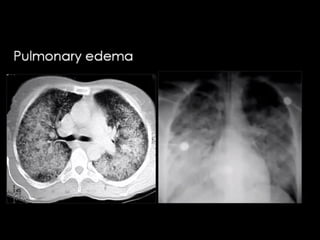
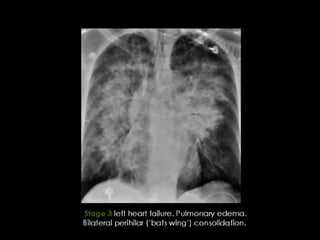
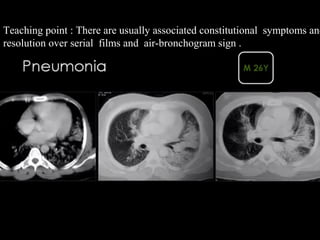
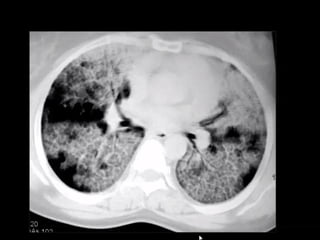
This document discusses various high attenuation patterns seen on CT scans of the lungs including ground glass opacity, consolidation, and their causes. It provides details on specific signs such as the dark bronchus sign seen with ground glass opacity and complete obscuration of vessels seen with consolidation. Various disease processes that can cause these findings are listed such as infection, chronic interstitial lung disease, and lung cancer.