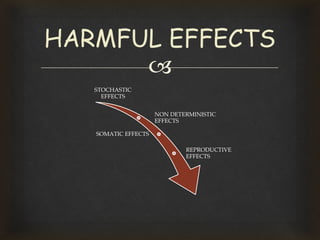
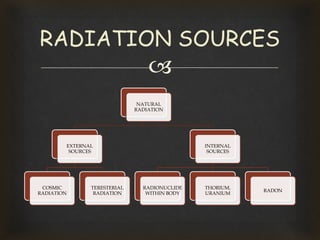
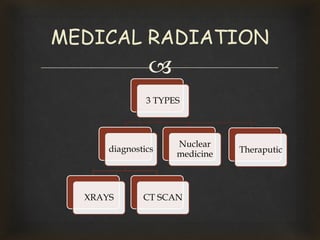
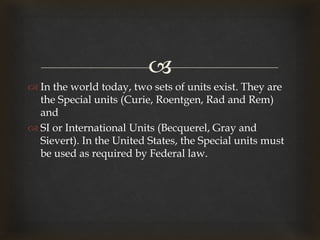
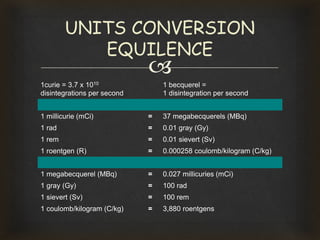
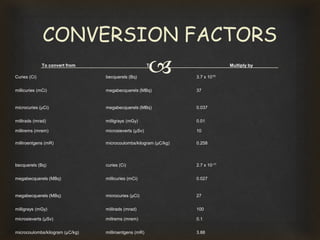
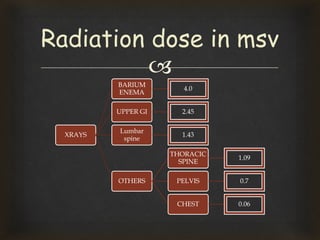
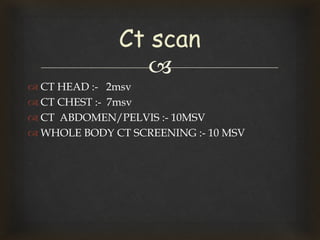
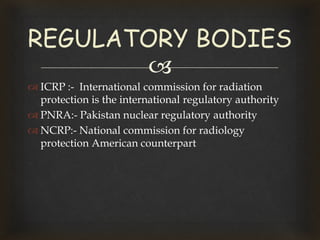
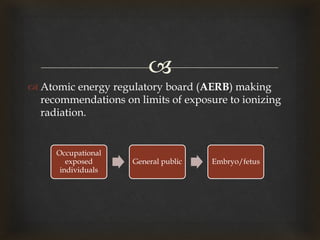
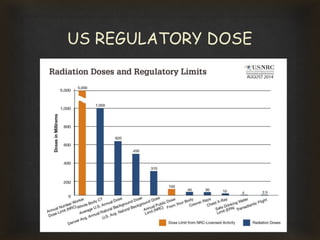
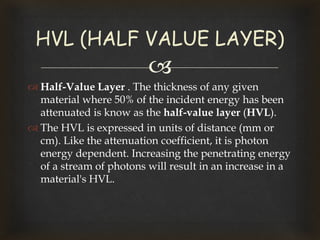
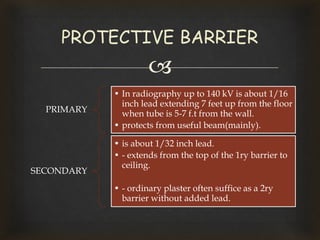
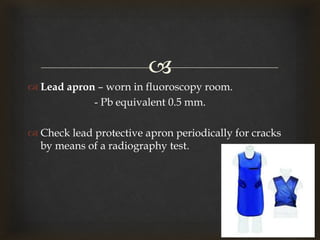
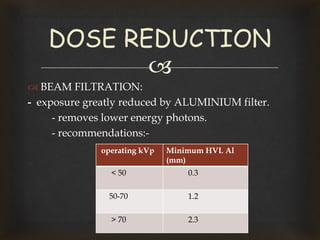
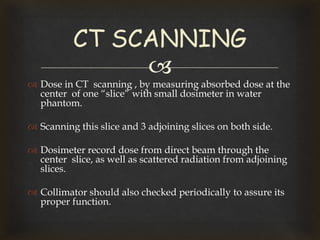
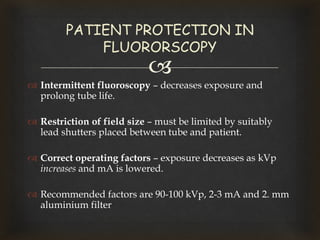
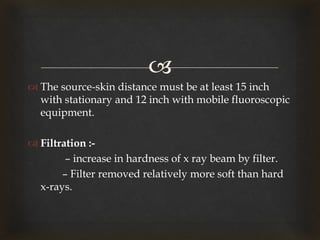
This document discusses radiation protection and provides definitions, types of radiation effects, sources of radiation exposure, units of measurement, dose limits, and techniques to reduce radiation exposure in medical imaging. It defines radiation protection as protecting people from harmful effects of ionizing radiation. It describes stochastic and deterministic effects and lists examples of radiation anomalies. It also outlines regulatory bodies, dose limits for occupational workers and the public, and principles of radiation safety including time, distance, shielding and reducing exposure.