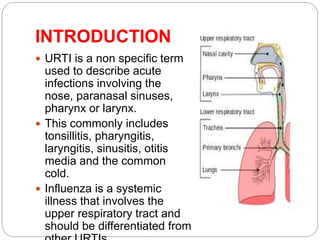
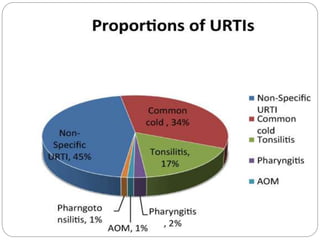
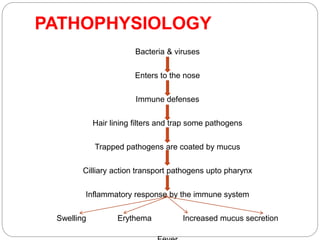
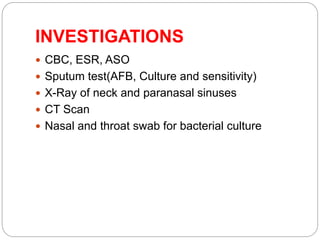
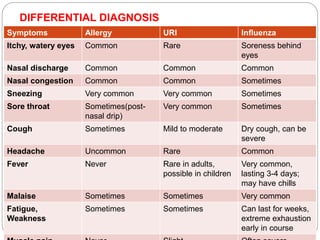
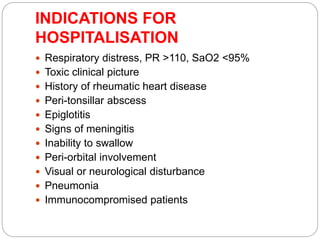
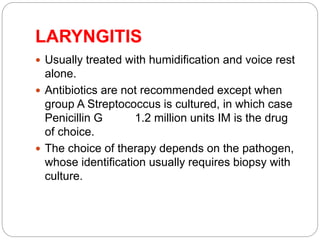
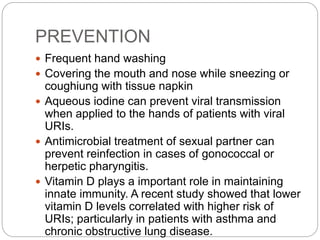
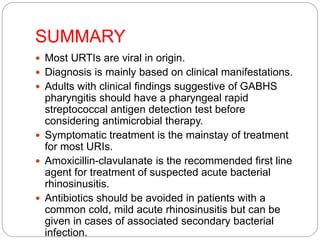
This document discusses upper respiratory tract infections (URTI). URTIs are commonly caused by viruses like rhinovirus, coronavirus, and influenza. They often involve the nose, sinuses, throat, and larynx, causing symptoms like nasal congestion, sore throat, cough. While most cases are viral, some bacterial infections like Streptococcus and Mycoplasma pneumoniae can also cause URTIs. Treatment involves rest, hydration, analgesics, and sometimes antibiotics for bacterial infections. Vaccines are recommended for influenza prevention.