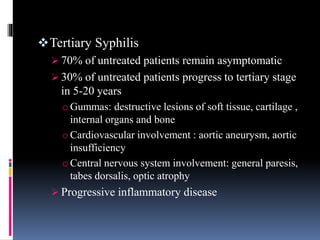
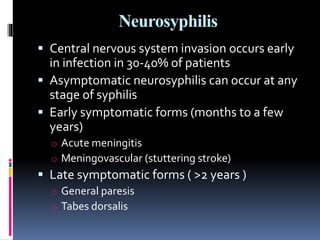
Syphilis is a bacterial infection spread through sexual contact or skin-to-skin contact with sores caused by the spirochete Treponema pallidum. It progresses through primary, secondary, latent, and tertiary stages if left untreated. Primary syphilis causes painless sores, usually on the genitals or mouth. Secondary syphilis symptoms include a rash, swollen lymph nodes, and general symptoms. Without treatment, syphilis can spread to the nervous system causing neurosyphilis. Diagnosis involves dark-field microscopy of sores or serological tests detecting antibodies. Penicillin is the treatment of choice and can cure syphilis if given early enough in the infection.