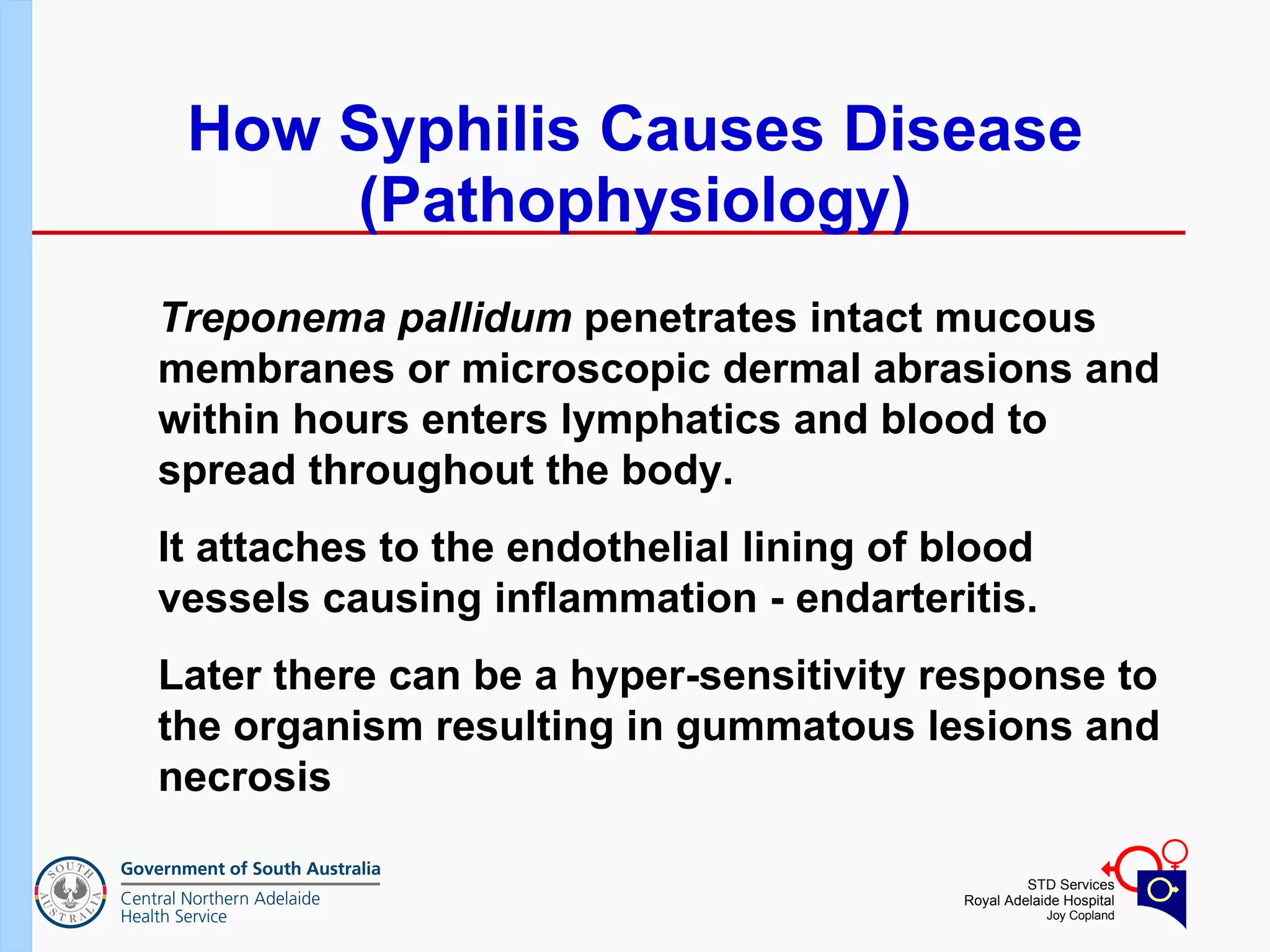
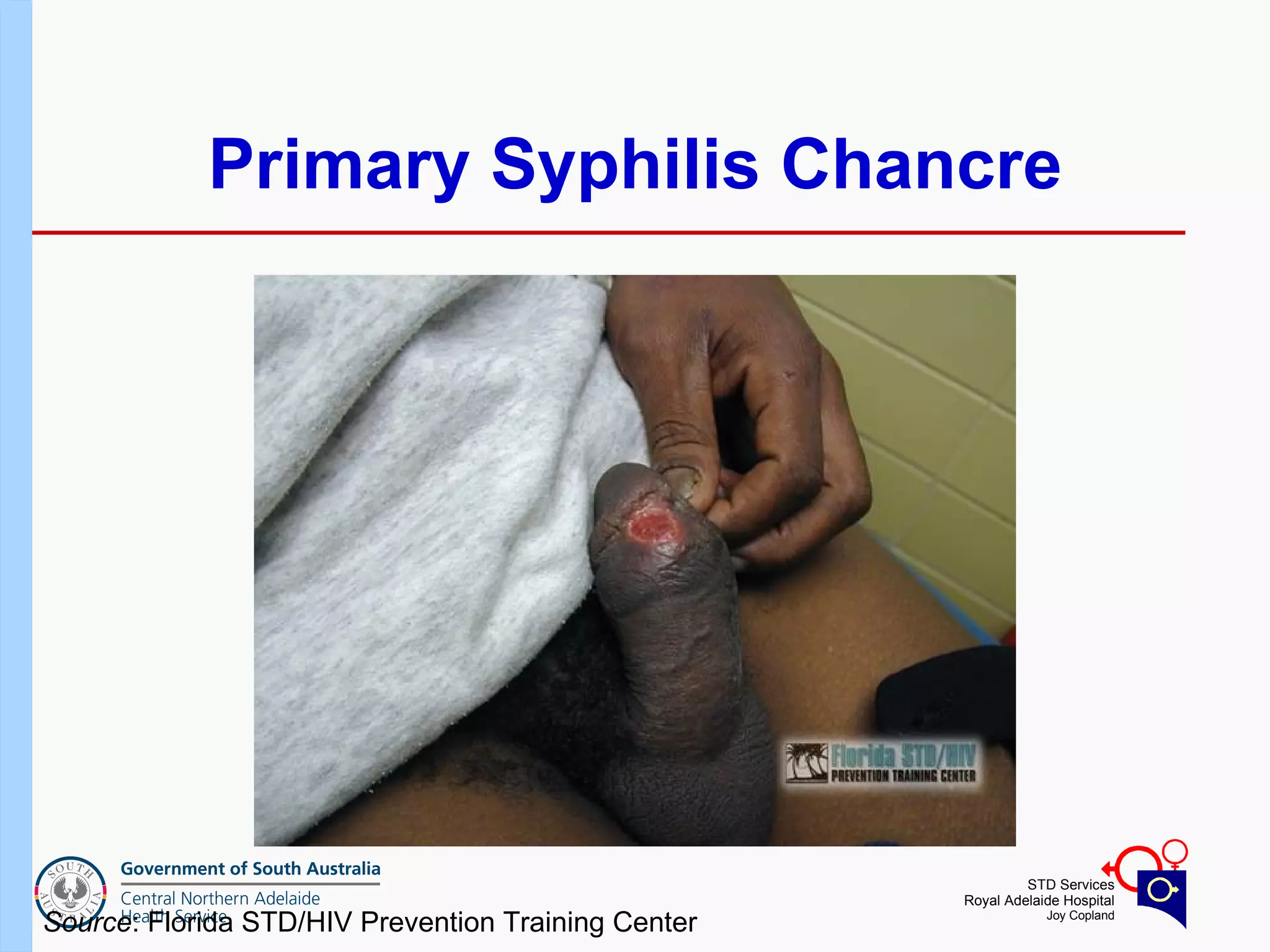
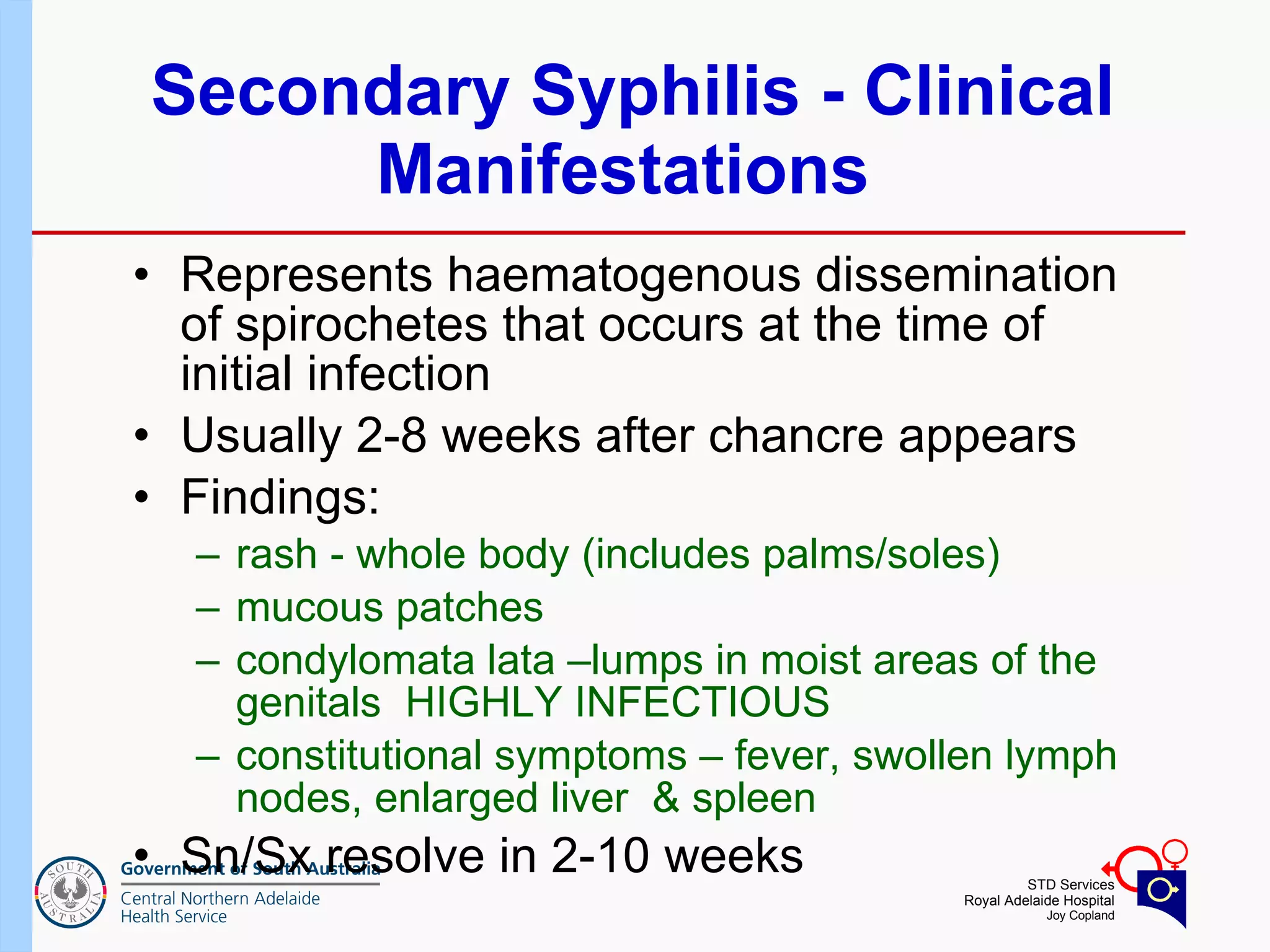
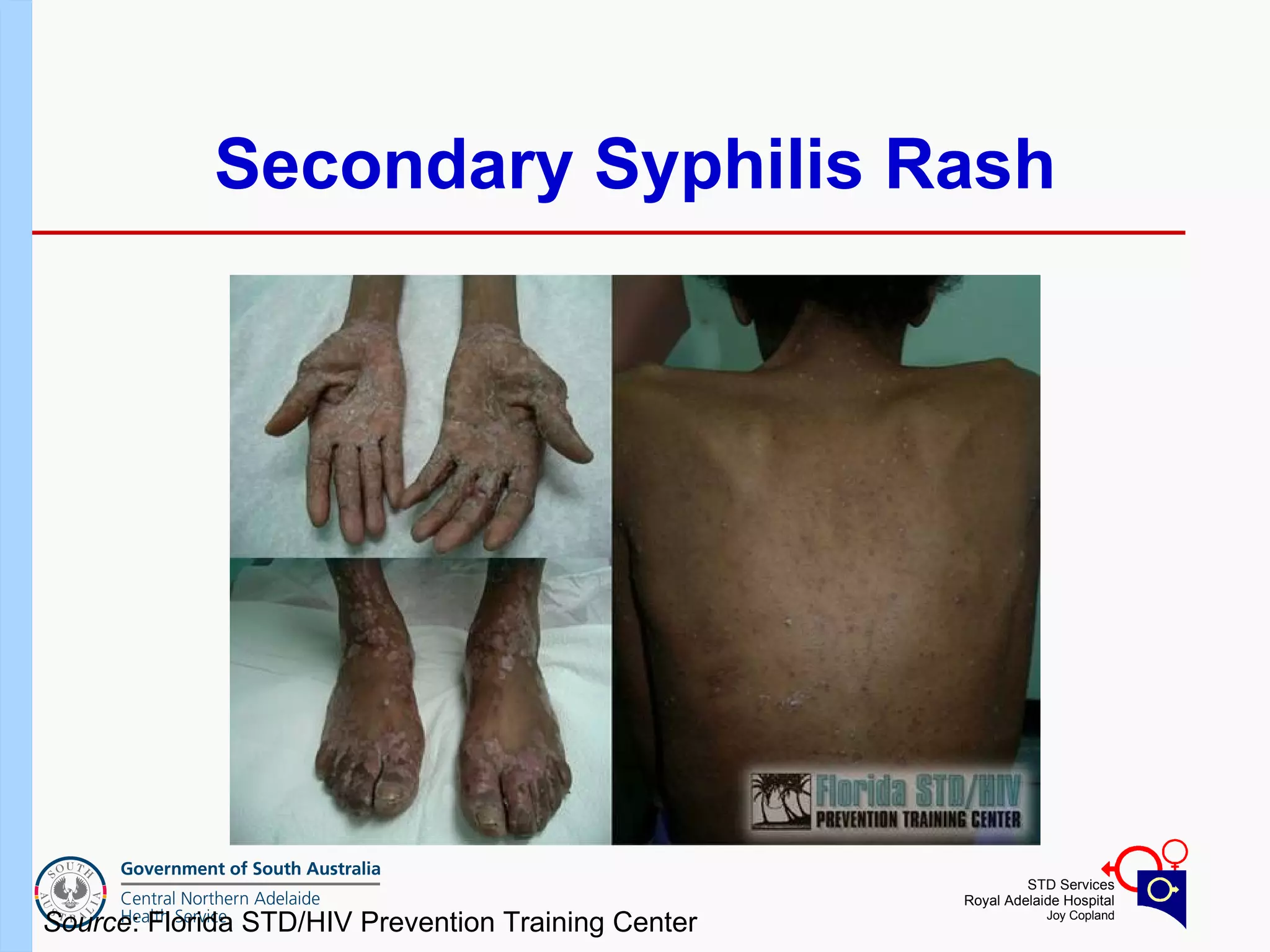
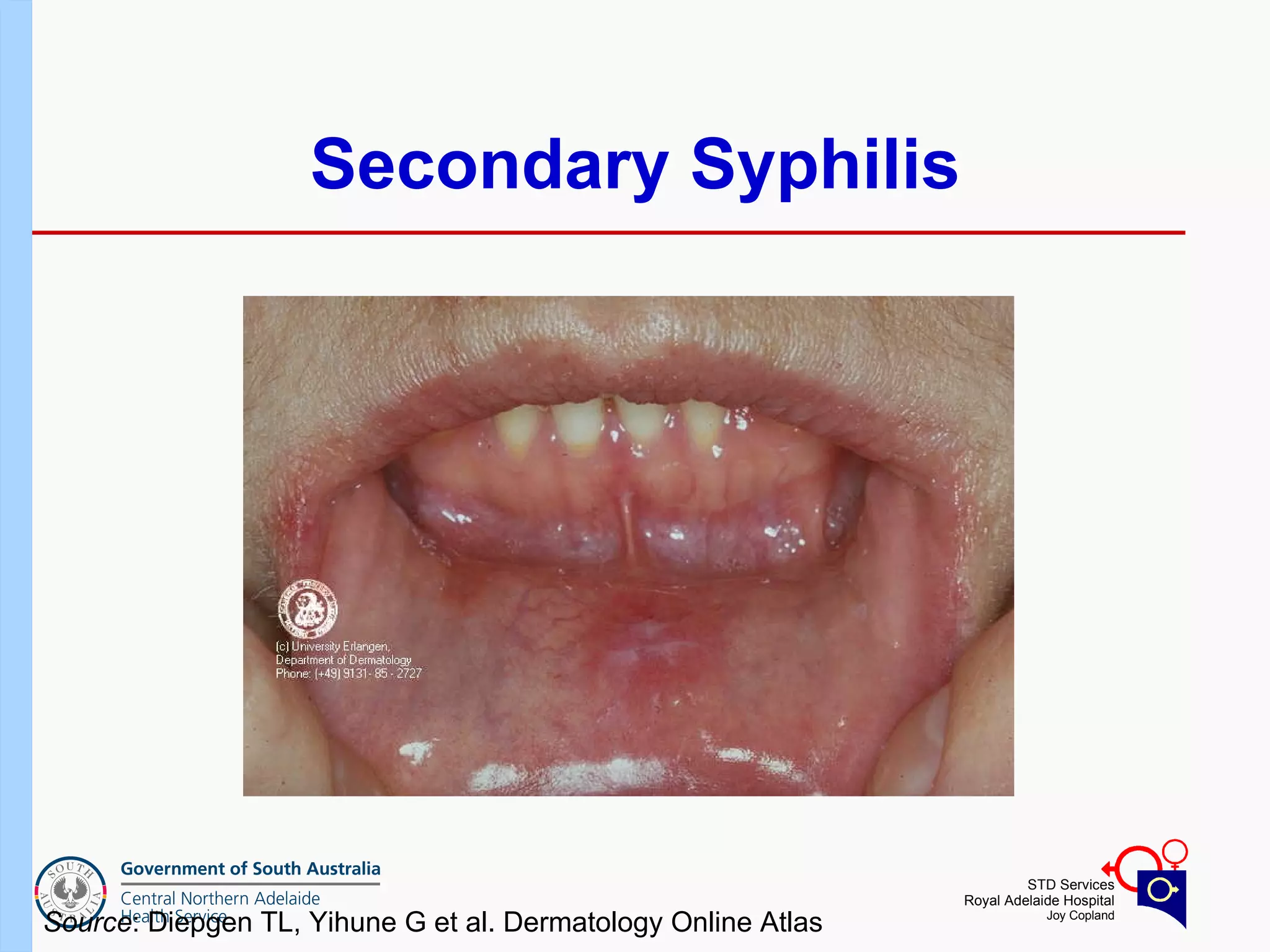
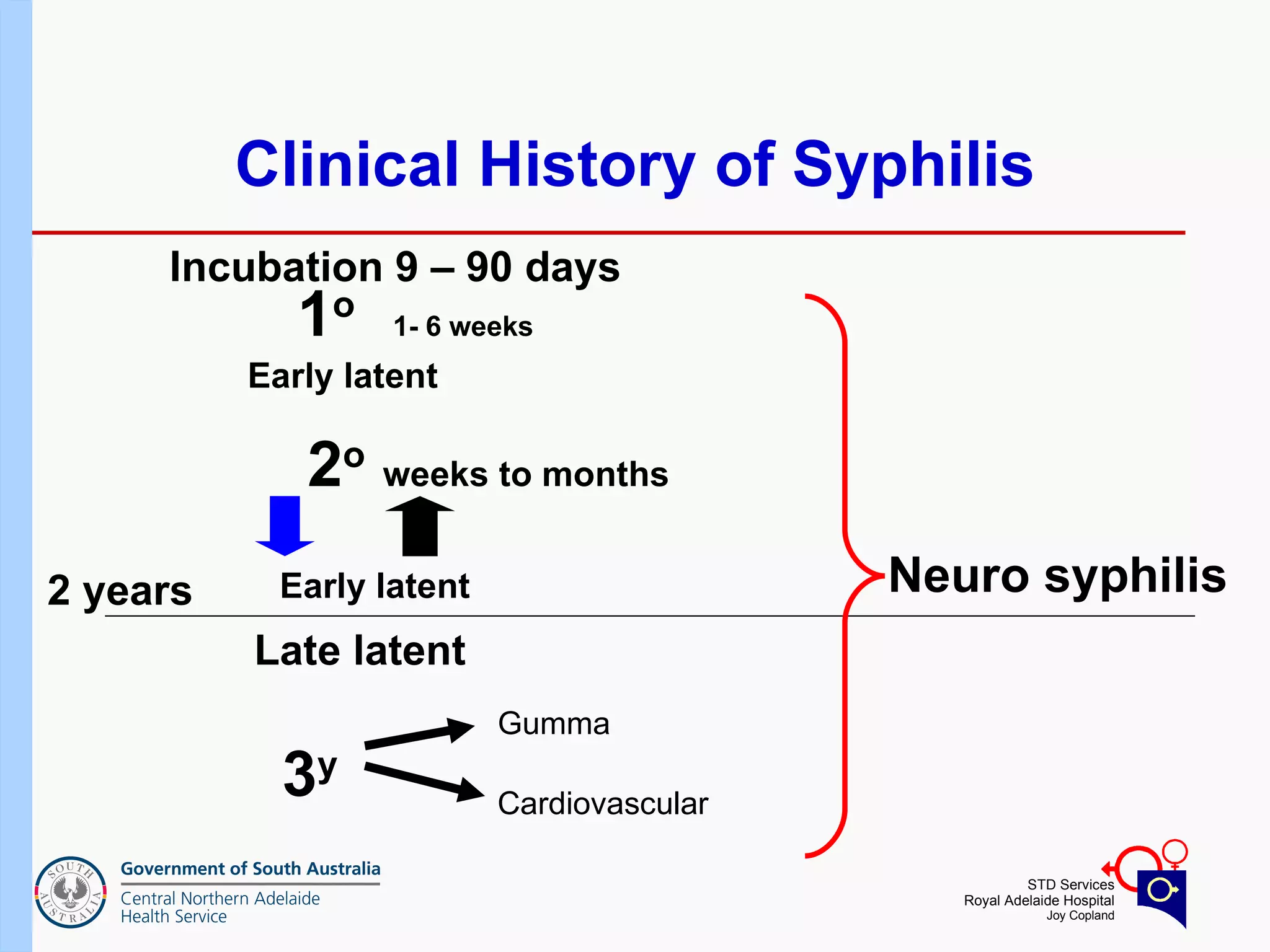
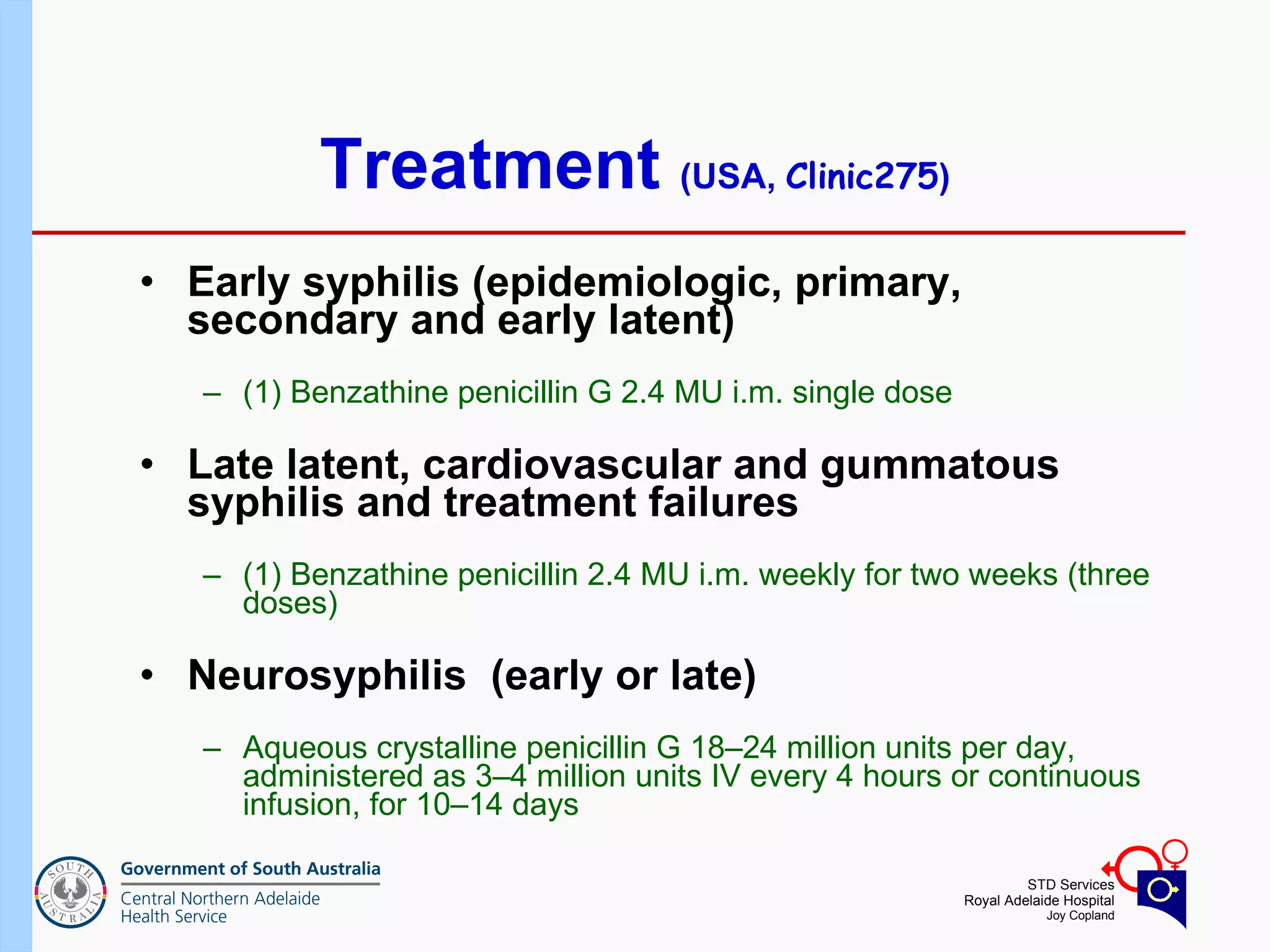
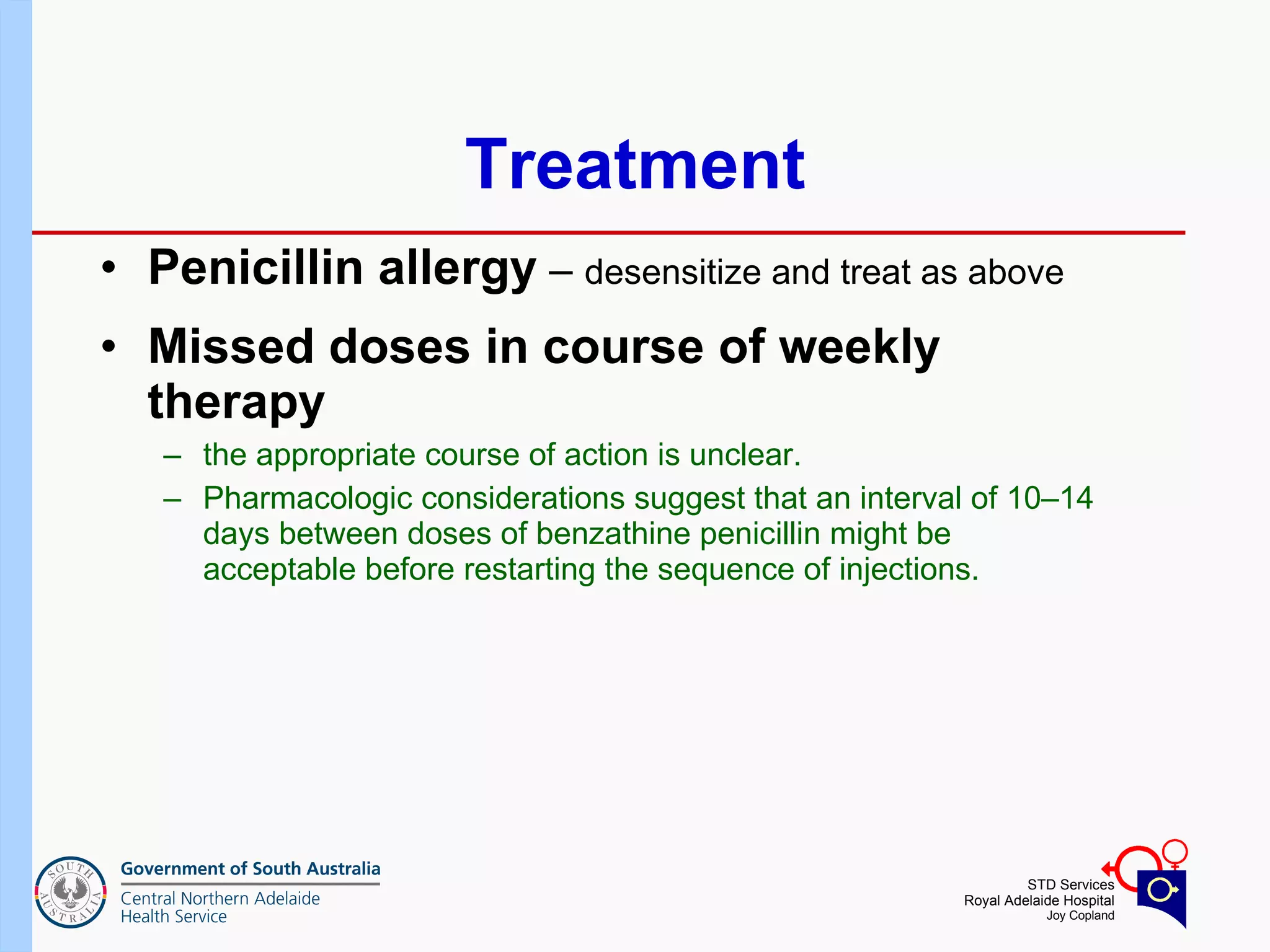
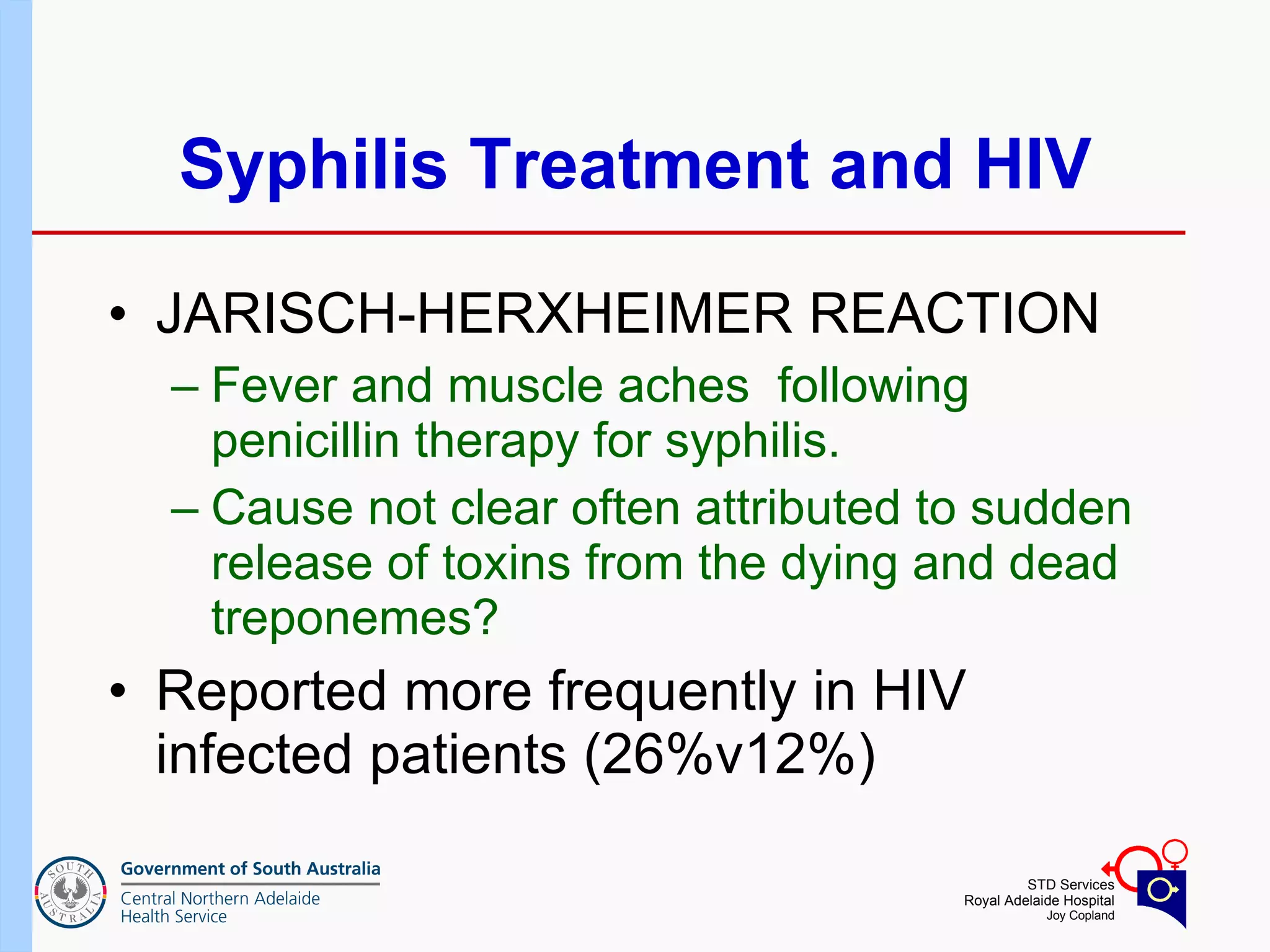
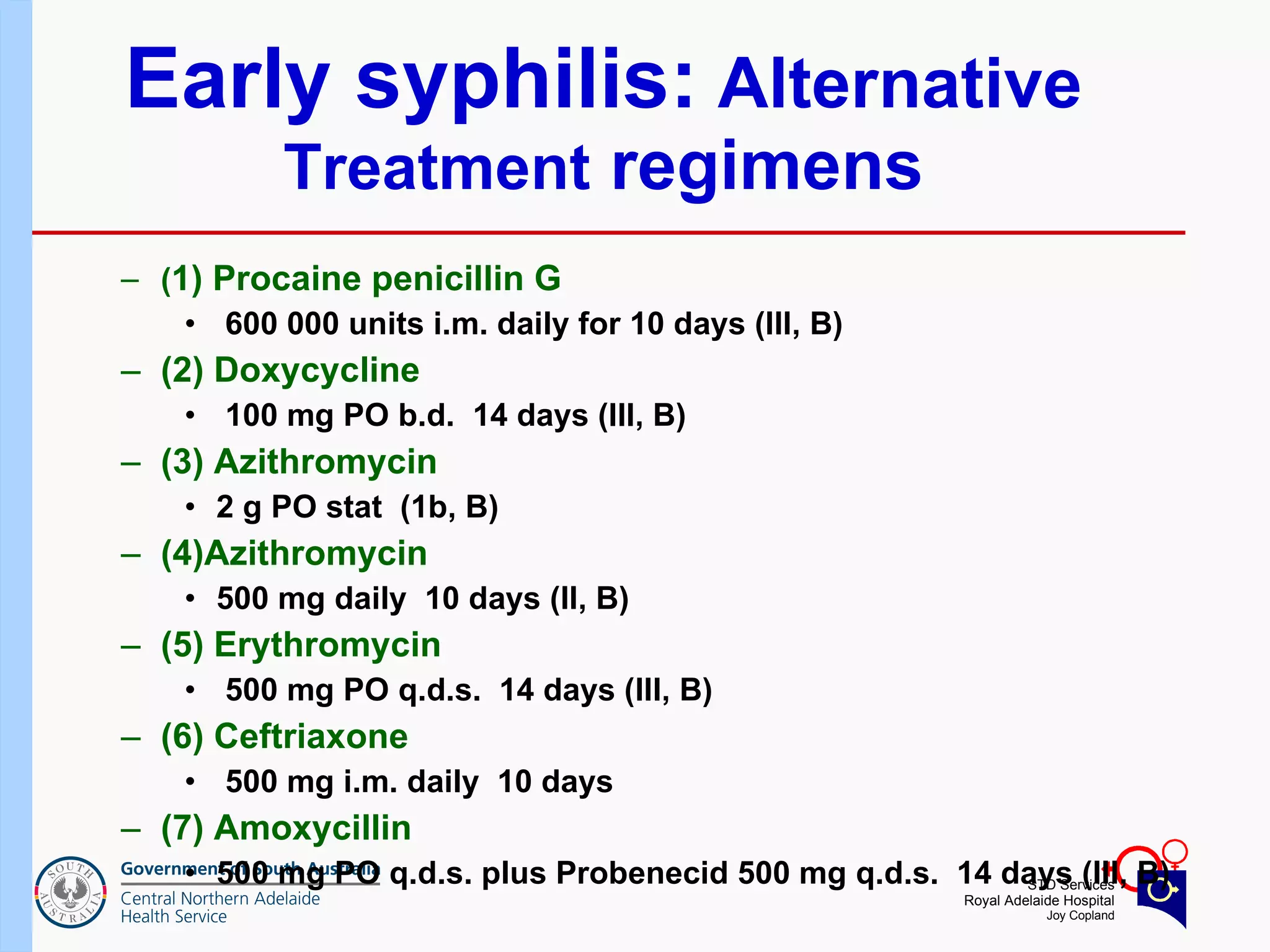
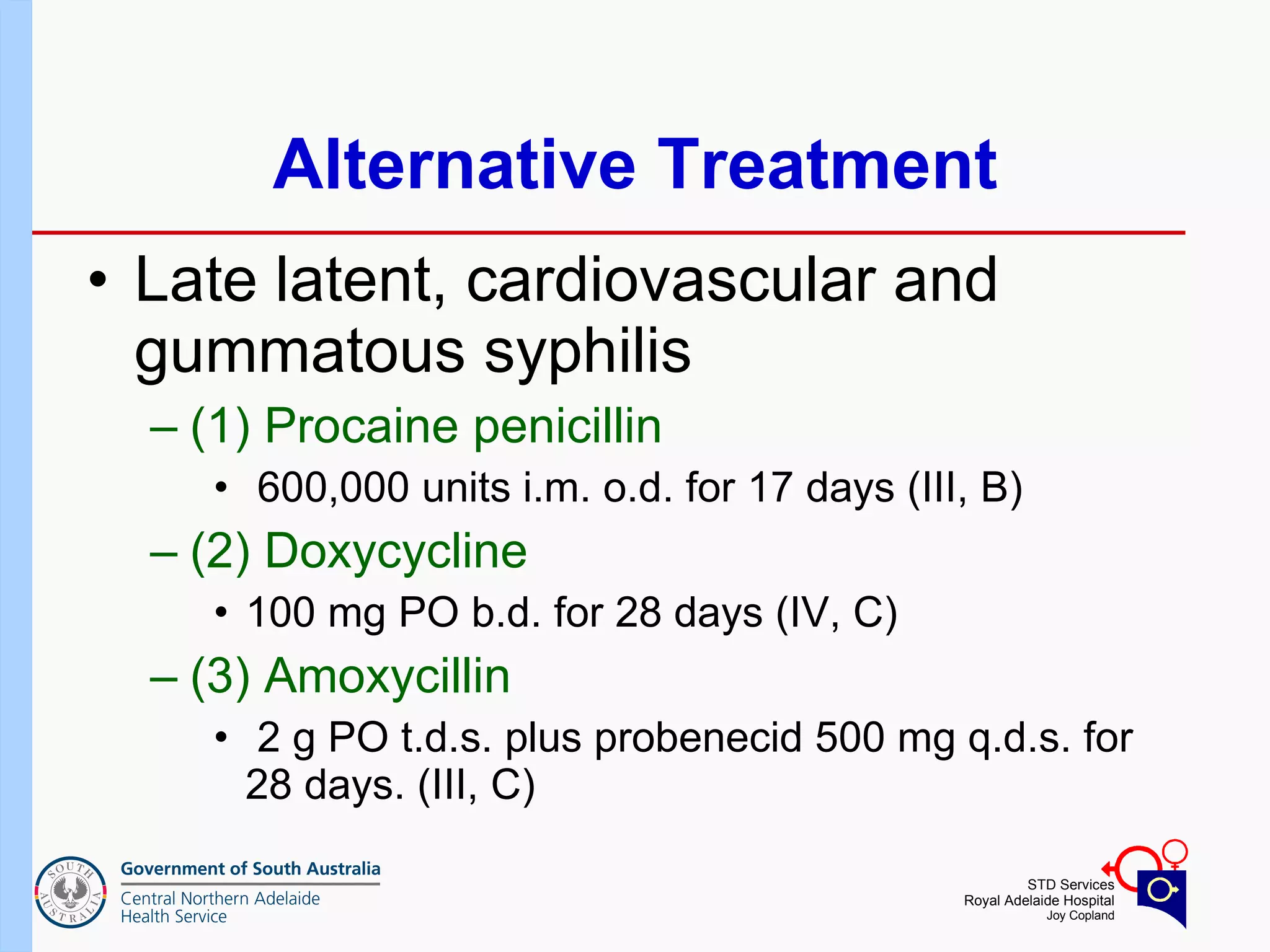
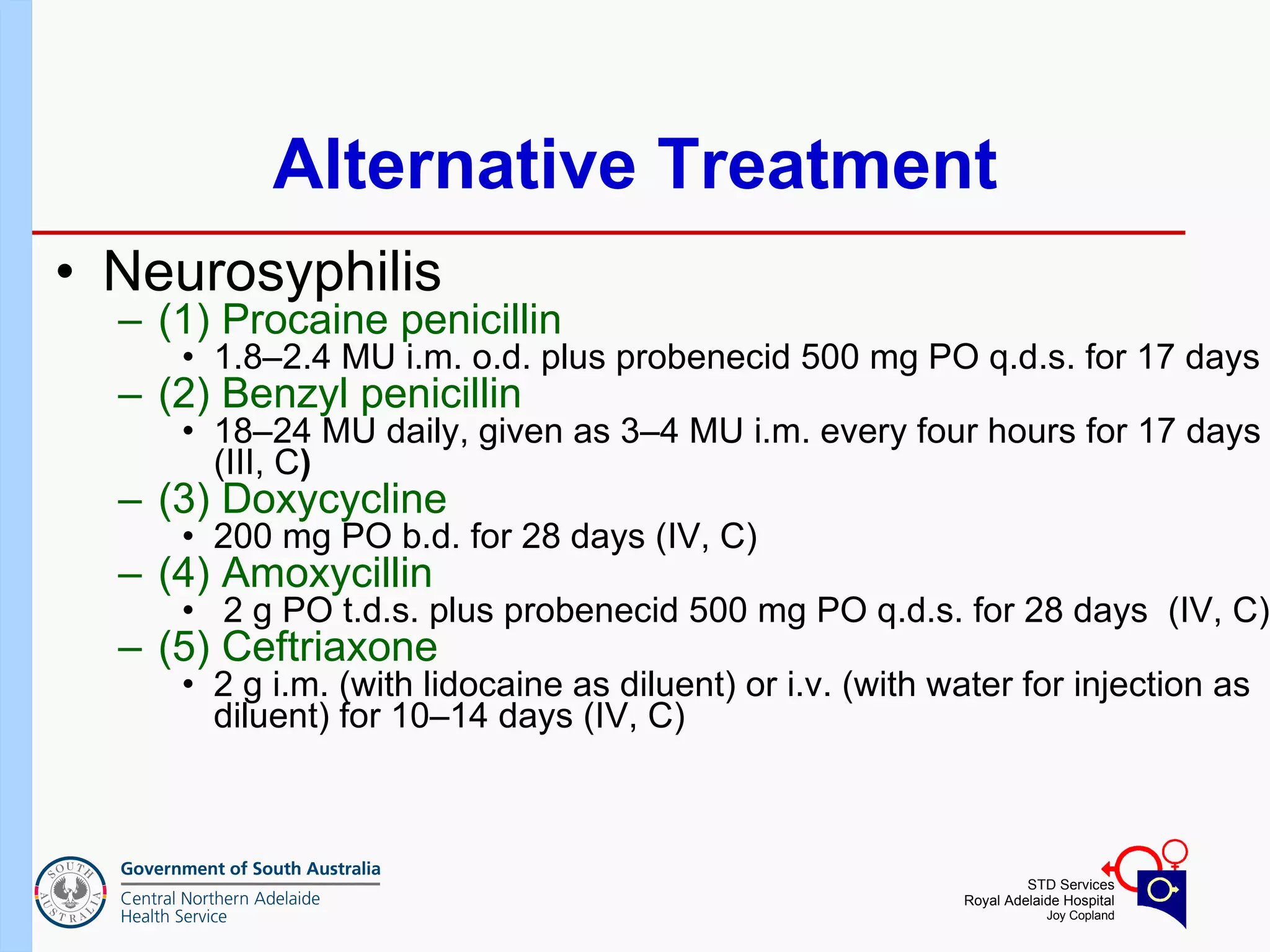
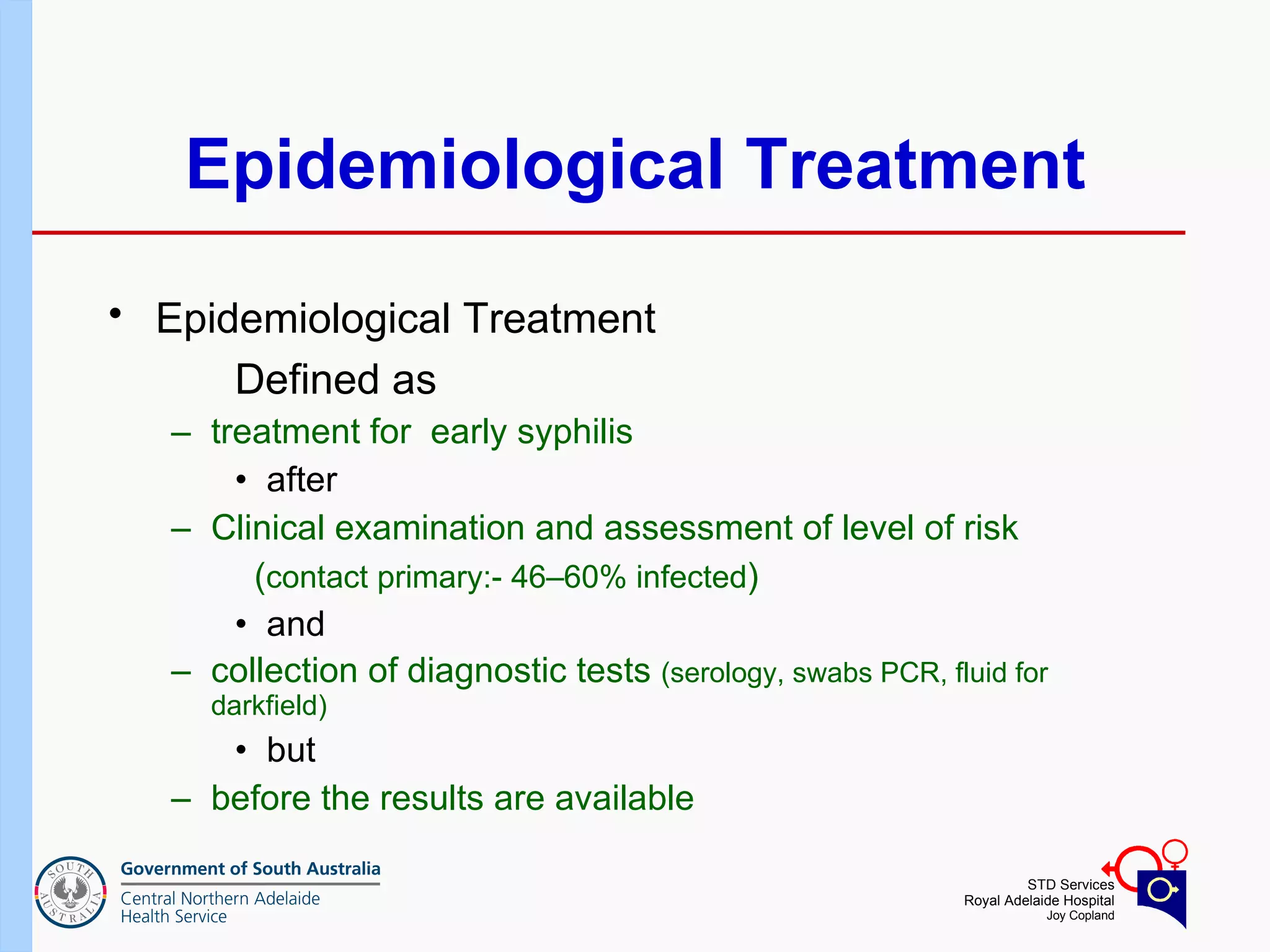
This document provides a detailed overview of syphilis, including its pathophysiology, clinical manifestations (primary, secondary, tertiary), and treatment protocols, especially in the context of HIV co-infection. It highlights the treatment regimens, the importance of serological testing, and considerations regarding the management of syphilis in HIV-positive patients. The document also discusses treatment failure, monitoring, and epidemiological treatment approaches for syphilis.
![Serological Tests in Untreated Syphilis *FTA-ABS and TP-PA are generally considered equally sensitive in the primary stage of disease. 100 100 93 EIA 73 98 (95-100) 100 86 (77-99) RPR 94 97 (97-100) 100 76 (69-90) TPPA* 96 100 100 84 (70-100) FTA-ABS* 71 (37-94) 95 (88-100) 100 78 (74-87) VDRL Tertiary Latent Secondary Primary Test Stage of Disease (Percent Positive [Range])](https://image.slidesharecdn.com/russellwaddell-syphilispresentationandtreatment-090622205332-phpapp01/75/Russell-Waddell-Syphilis-Presentation-and-Treatment-34-2048.jpg)