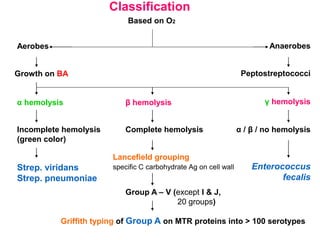
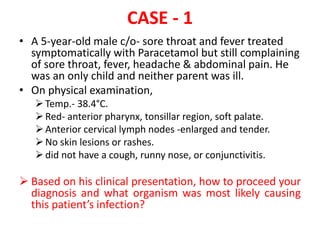
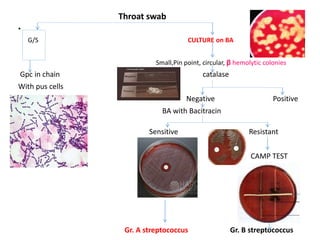
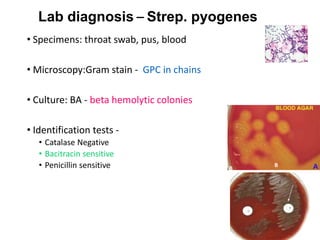
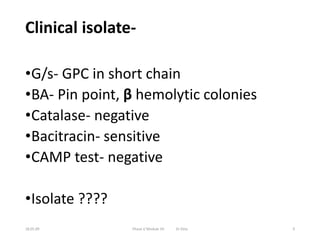
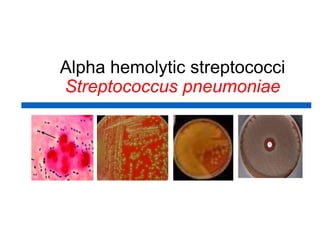
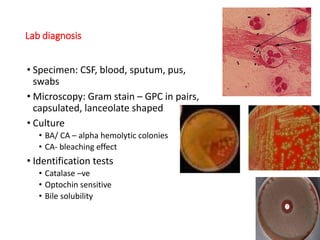
This document discusses the laboratory diagnosis of various Streptococcus species based on their characteristics and test results. It describes how S. pneumoniae can be identified from other alpha-hemolytic streptococci based on being catalase-negative, optochin-sensitive, and bile soluble. It also discusses how S. pyogenes causing a sore throat in a child can be identified as the cause based on being a beta-hemolytic streptococcus that is catalase-negative and bacitracin-sensitive. For the patient with pneumonia, S. pneumoniae is identified as the likely pathogen from alpha-hemolytic colonies that are catalase-negative and optochin-sensitive in sputum culture.