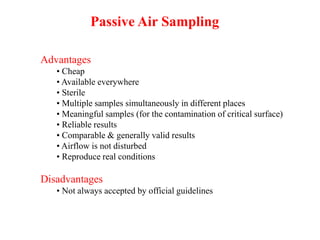
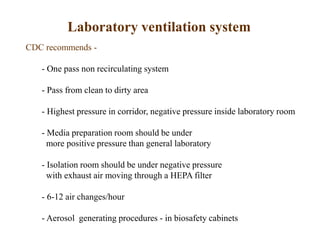
This document discusses bacteria in air and methods of air sampling. It notes that air is a mixture of gases with typical composition by volume being nitrogen 78%, oxygen 20.93%, and trace amounts of other gases. Indoor air undergoes physical and chemical changes from factors like temperature, humidity, and metabolic processes. Bacteria are present in all air and can be transmitted person-to-person in aerosols. The size of particles impacts where they are deposited in the respiratory system. Various methods are described for sampling and quantifying bacteria in air, as well as strategies to control airborne bacteria like isolation systems, air filtration, UV irradiation, and engineering controls.