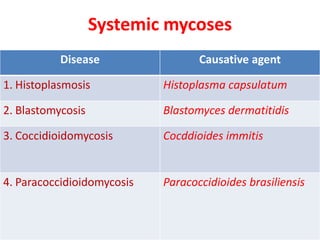
1. The document describes four systemic mycoses caused by dimorphic fungi: histoplasmosis, blastomycosis, coccidioidomycosis, and paracoccidioidomycosis.
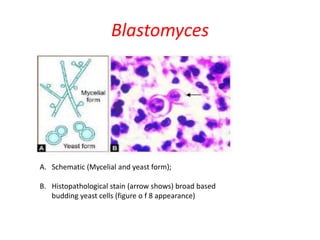
2. It provides details on the causative agents, pathogenesis, clinical manifestations, laboratory diagnosis including histopathology, culture, and serology, and treatment recommendations for each fungal infection.
3. Key diagnostic methods include histopathological staining of tissue samples to identify characteristic fungal structures, culture of samples to demonstrate the dimorphic nature of the fungi, and serological tests to detect antibodies.