1) Sterilization is a process that eliminates all microorganisms, while disinfection only eliminates pathogens.
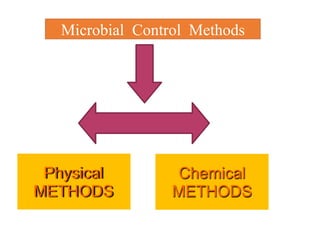
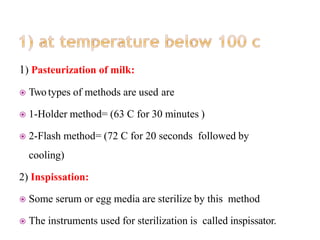
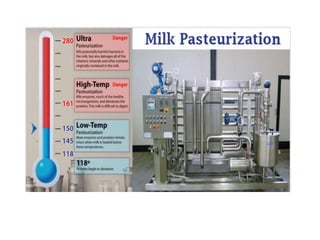
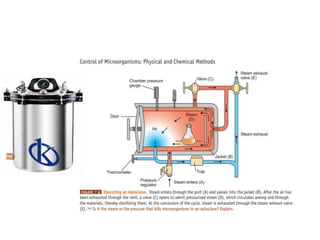
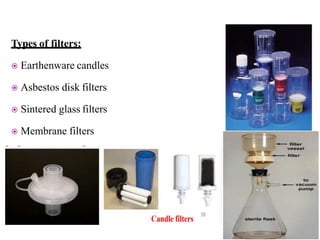
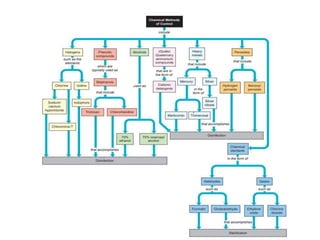
2) Physical sterilization methods include heat, radiation, filtration, and sunlight. Heat sterilization can be dry or moist. The autoclave uses moist heat under pressure.
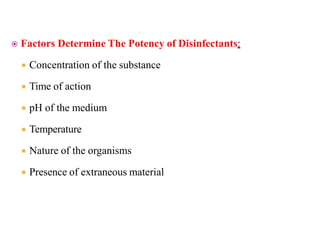
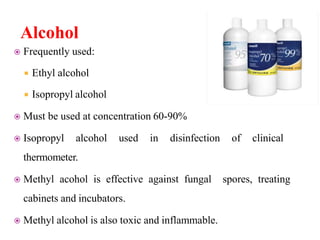
3) Chemical sterilization agents include alcohols, aldehydes, phenols, halogens, dyes, and gases. Their effectiveness depends on concentration, contact time, temperature, and other factors. Common disinfectants are alcohol, formaldehyde, iodine, chlorine, and phenol-based compounds.