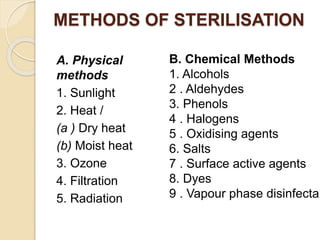
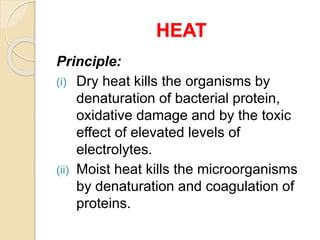
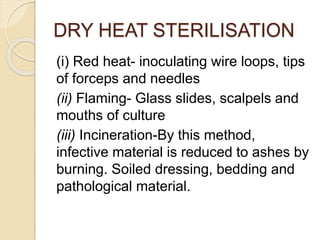
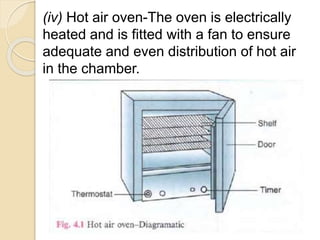
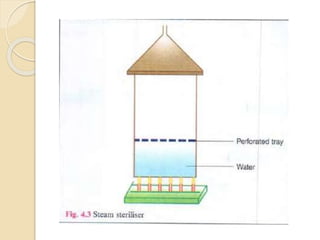
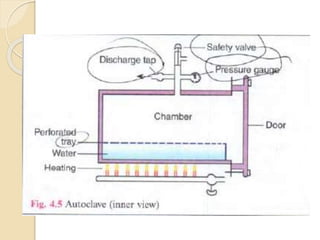
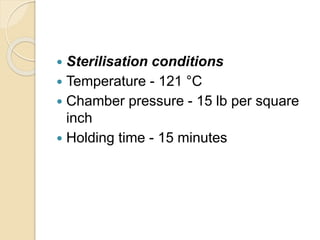
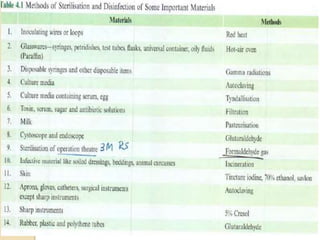
This document summarizes sterilization and disinfection methods. It discusses sterilization as a process that eliminates all microorganisms, while disinfection only eliminates pathogens. Physical sterilization methods include heat, radiation, and filtration. Heat sterilization can be achieved through dry heat or moist heat above 100°C using an autoclave. Chemical disinfectants include alcohols, aldehydes, phenols, and halogens. An ideal disinfectant is broad-spectrum, fast-acting, stable, non-toxic, and inexpensive. Factors like concentration, temperature, and organic matter influence disinfectant potency.