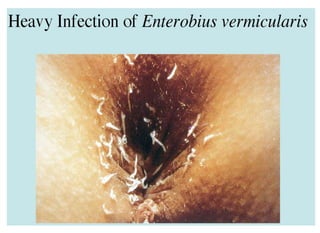
Enterobius vermicularis, also known as the pinworm or threadworm, is a parasitic nematode that infects the large intestine of humans. It has a worldwide distribution. The adult worms inhabit the cecum and ascending colon, where mating occurs. The female migrates to the perianal area at night to lay eggs, causing pruritus. Diagnosis is made by detecting eggs on perianal tape or swab samples under microscopy. Treatment involves a single dose of anthelmintic drugs like pyrantel pamoate or mebendazole. Personal hygiene measures and treating infected family members can aid prevention.