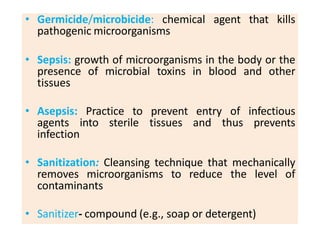
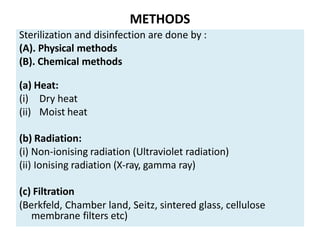
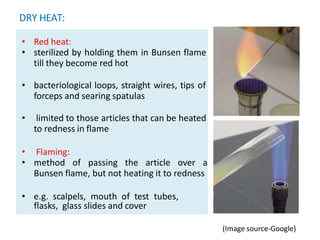
The document provides a comprehensive overview of sterilization and disinfection methods in microbiology, detailing definitions and applications of sterilization, disinfection, antisepsis, and related terms. It outlines various physical and chemical methods of sterilization, including heat, radiation, filtration, and specific techniques like pasteurization and autoclaving. Important factors affecting sterilization efficacy, such as temperature, time, and microbial resistance, are also discussed.