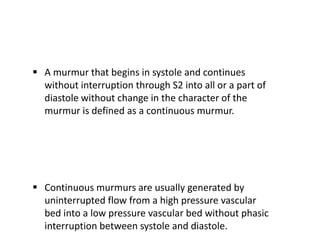
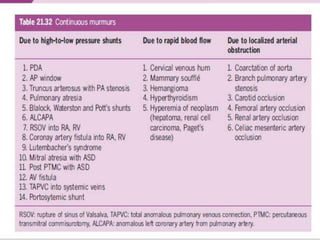
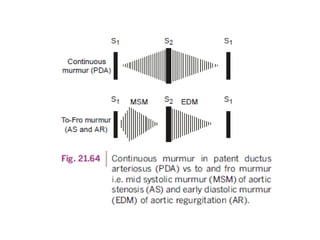
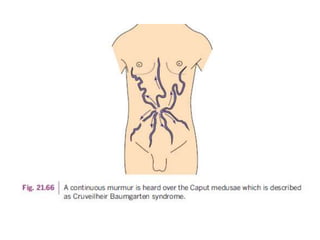
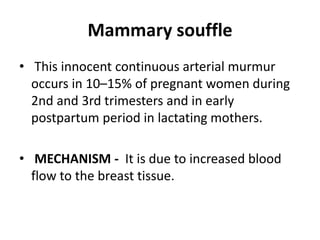
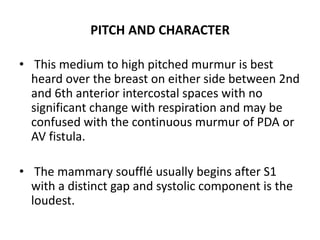
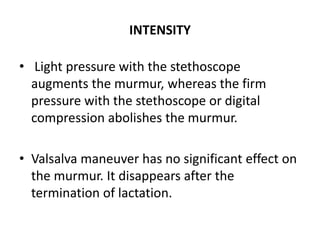
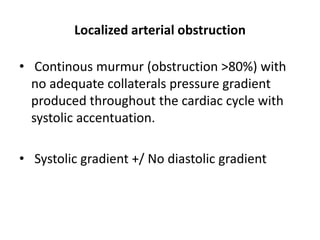
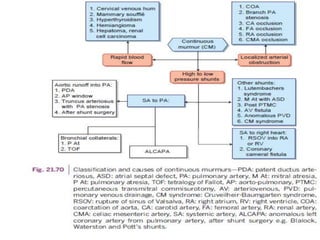
This document discusses continuous murmurs, which are murmurs that begin in systole and continue uninterrupted through diastole. The main causes of continuous murmurs are high to low pressure shunts, such as a patent ductus arteriosus (PDA) or ruptured sinus of valsalva. Continuous murmurs can also be caused by rapid blood flow, such as in hyperthyroidism. The document describes the characteristics, locations, and distinguishing features of continuous murmurs from various underlying conditions.