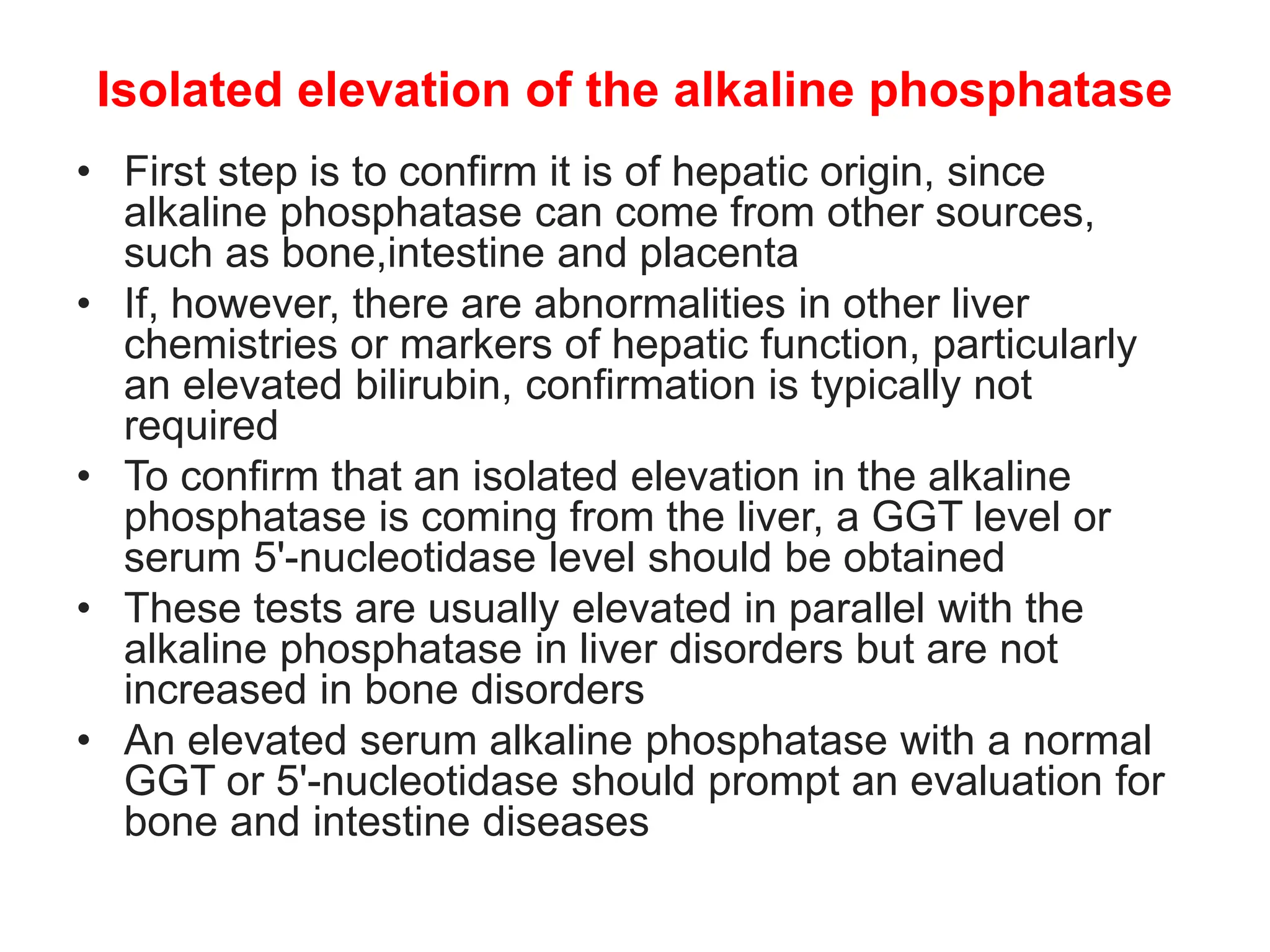
The document outlines the significance and interpretation of liver function tests, including serum aminotransferases, bilirubin, alkaline phosphatase, albumin, and prothrombin time, which indicate liver health and various liver diseases. It discusses test patterns associated with hepatocellular injury, cholestasis, and other conditions, along with their biochemical implications. Additionally, it details the evaluation process for elevated alkaline phosphatase and bilirubin levels, emphasizing the diagnostic pathways for hepato-biliary disorders.







![• Causes of elevated AST and ALT
• Liver disease
• Serum aminotransferases are elevated in most liver diseases and in
disorders that involve the liver (such as various infections, metabolic
dysfunction-associated steatotic (fatty) liver disease [MASLD], acute
and chronic heart failure, and metastatic carcinoma)
• Other conditions associated with elevated and low enzymes
• Drugs such as erythromycin and furosemide may produce falsely
elevated aminotransferase
• In contrast, falsely low serum AST (but not ALT) is seen in persons with
renal failure or those taking isoniazid
• In persons with renal failure, serum AST activity increases significantly
after hemodialysis, indicating removal of an inhibitor, which does not
appear to be urea
• Subnormal values of serum ALT have been described in patients with
Crohn disease, the reason for which is unclear
• Consumption of coffee and especially caffeine may lower serum ALT
and AST levels by mechanisms that are incompletely understood](https://image.slidesharecdn.com/liverfunctiontests-240522100059-9cd5358b/75/liver-function-tests-interpretation-pptx-11-2048.jpg)