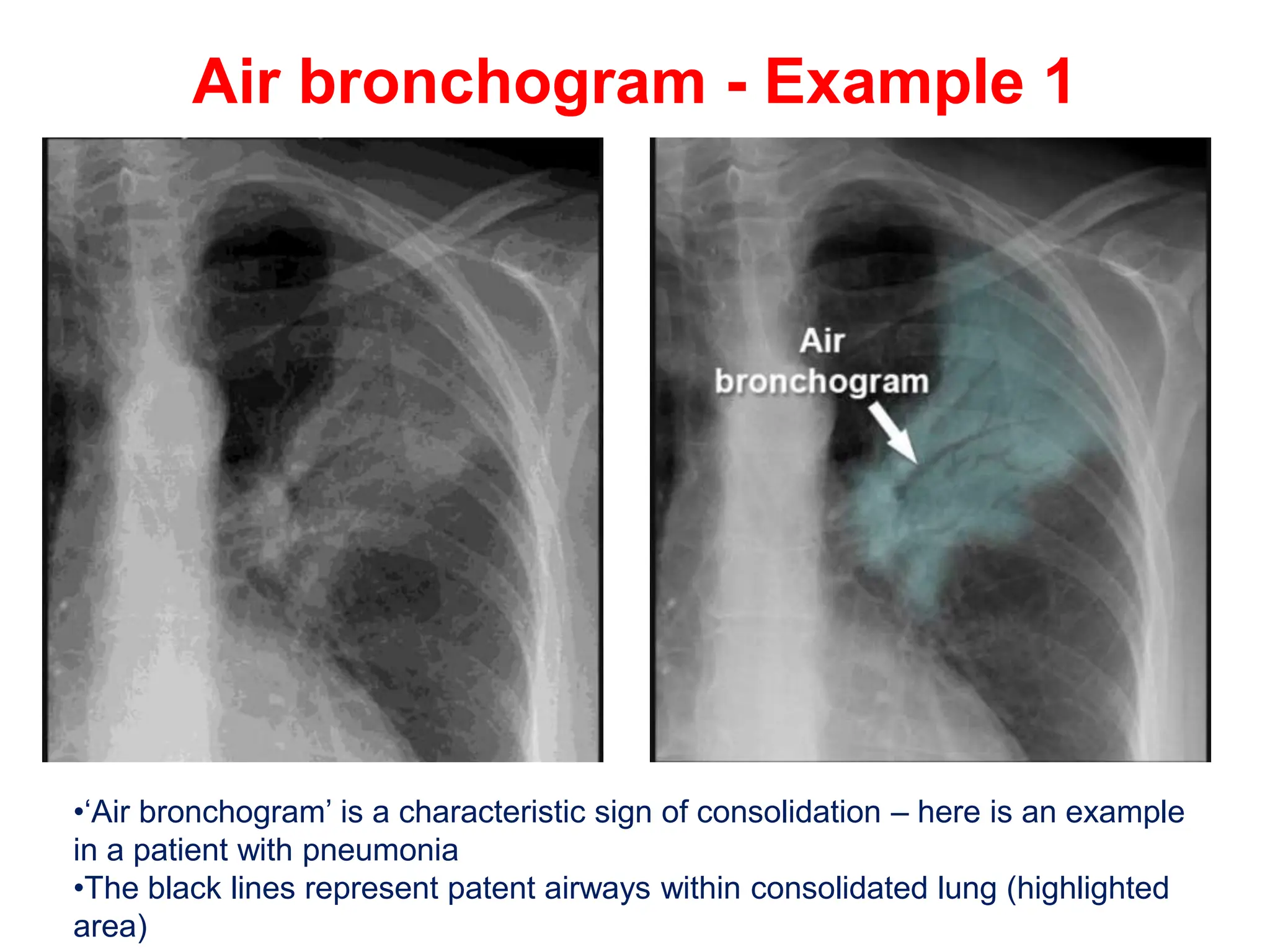
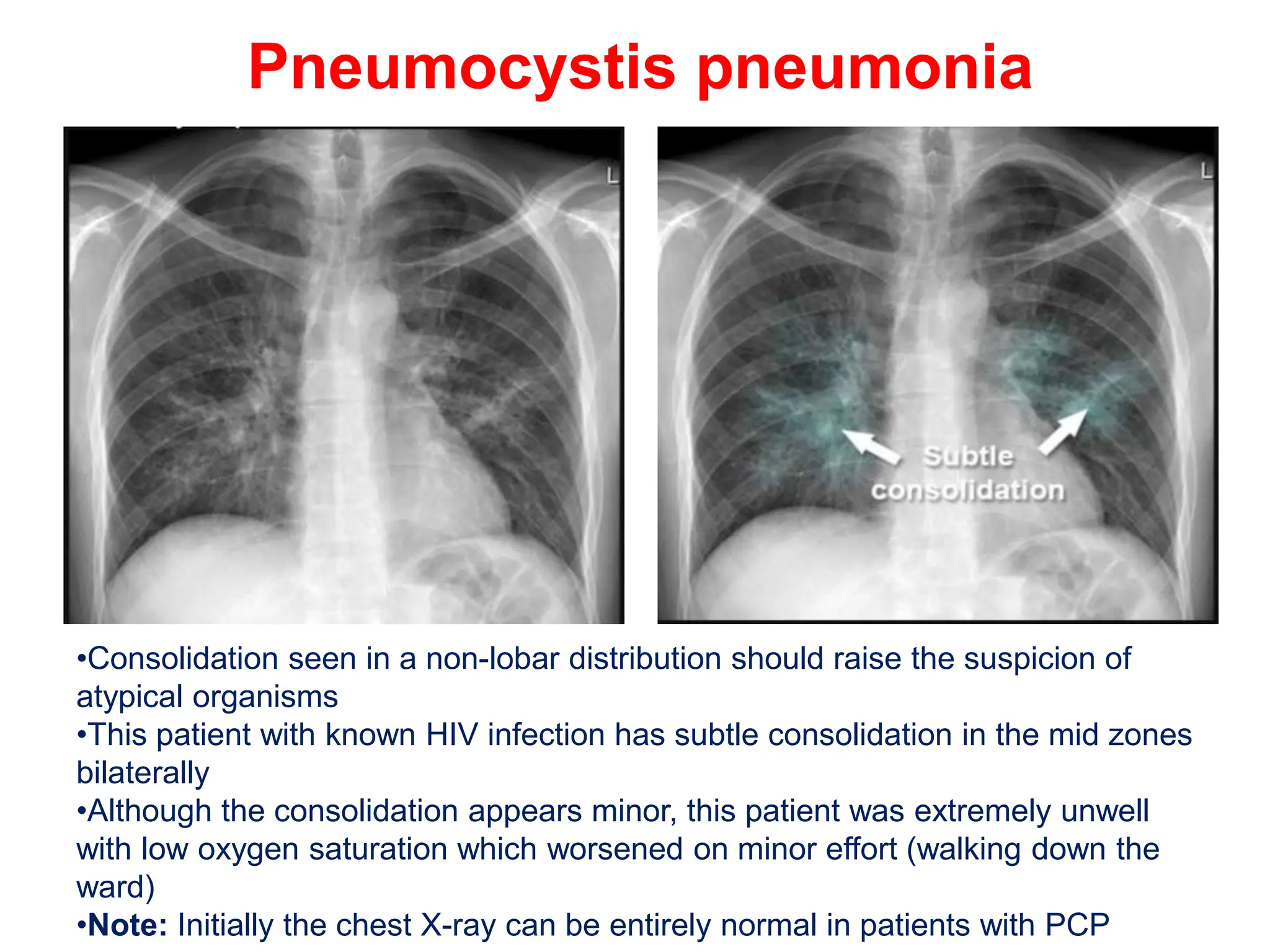
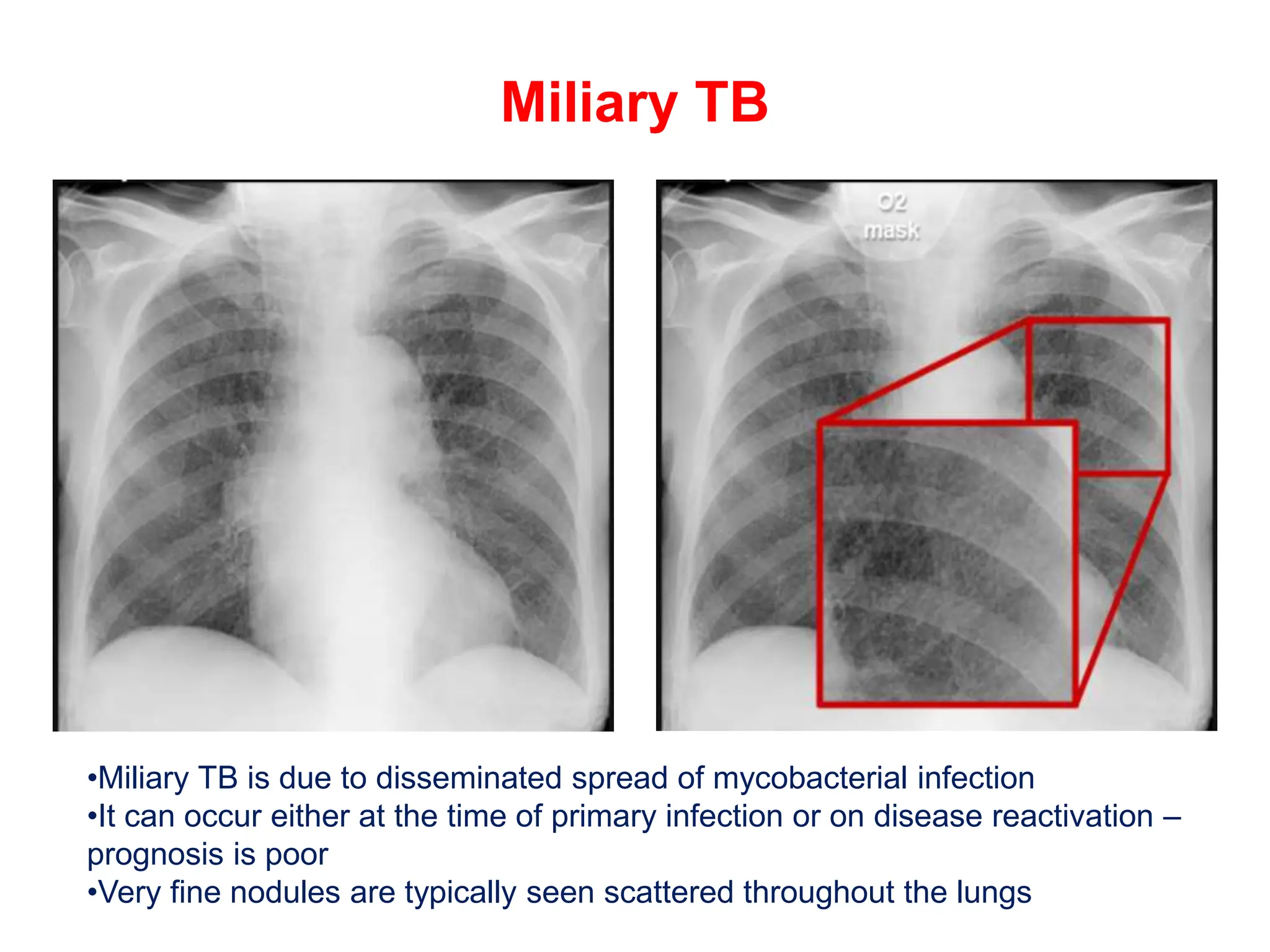
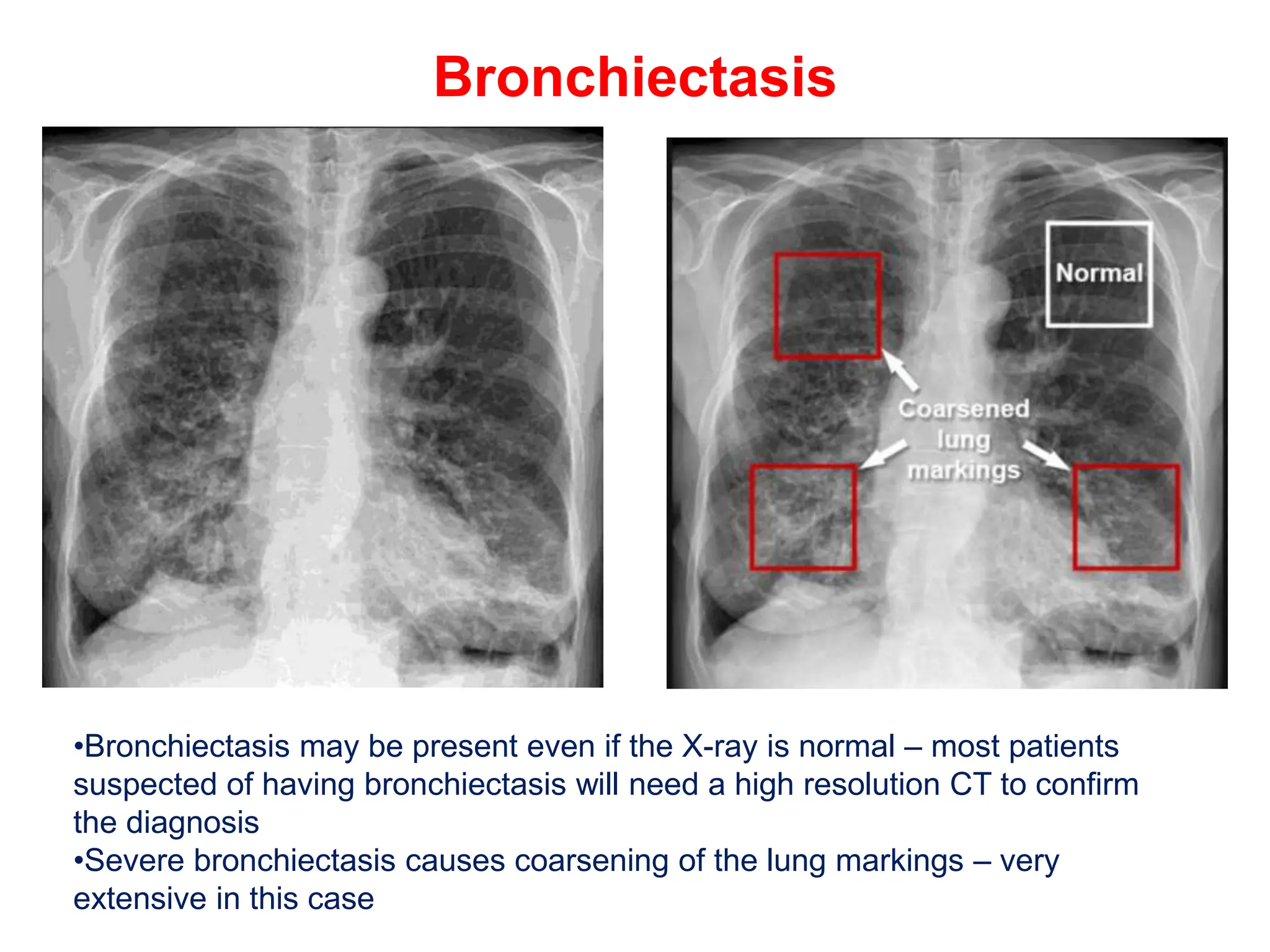
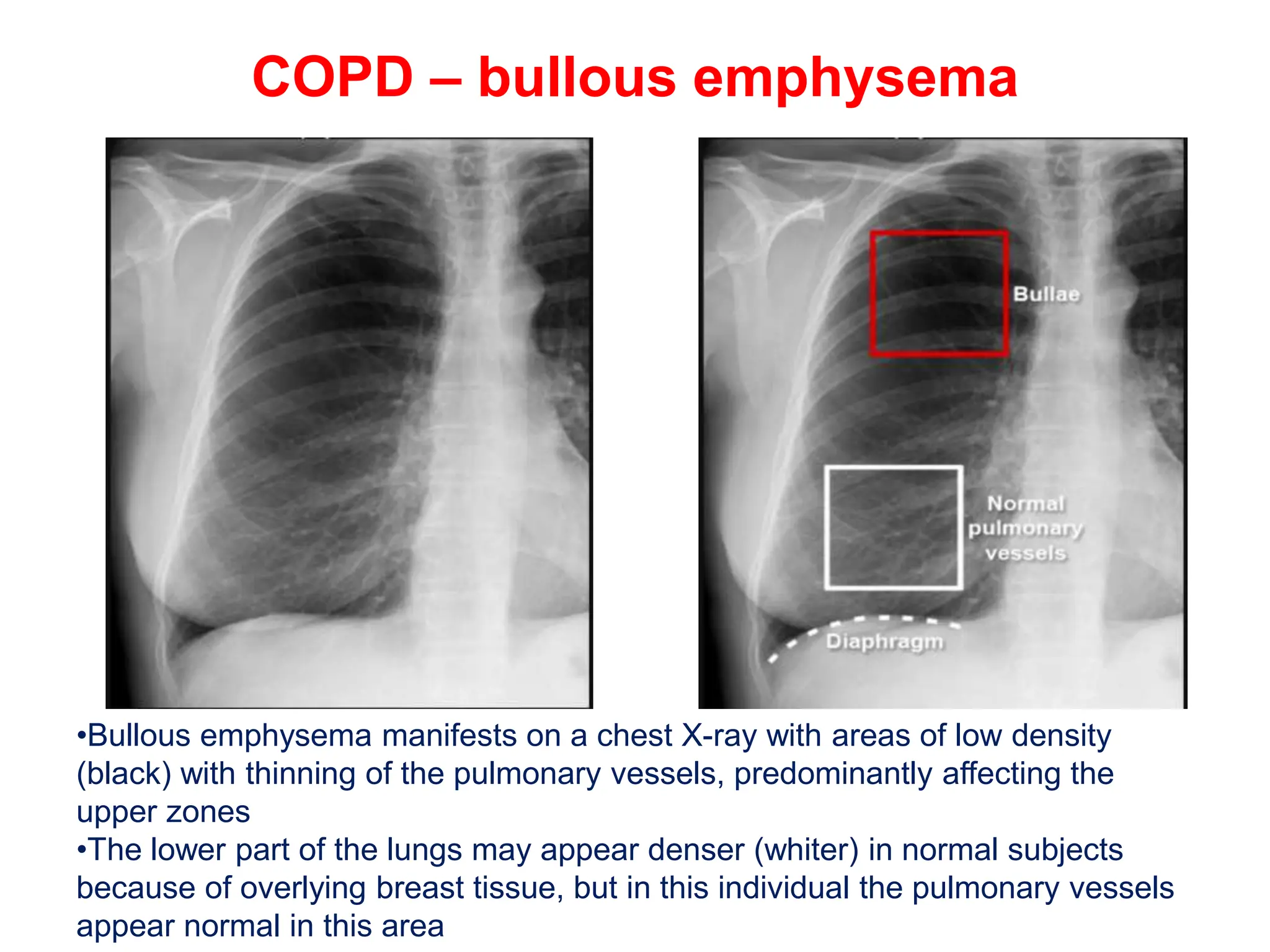
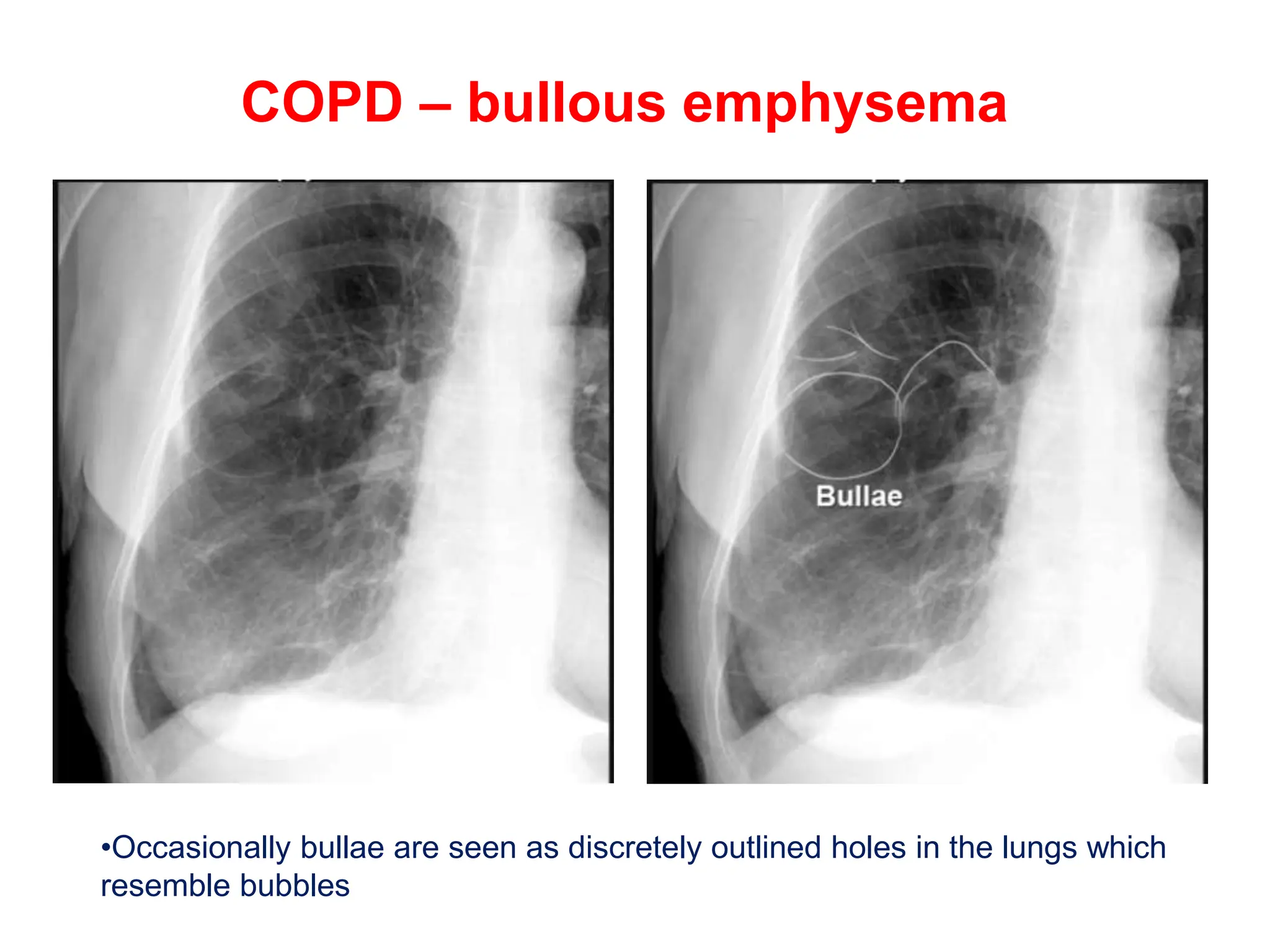
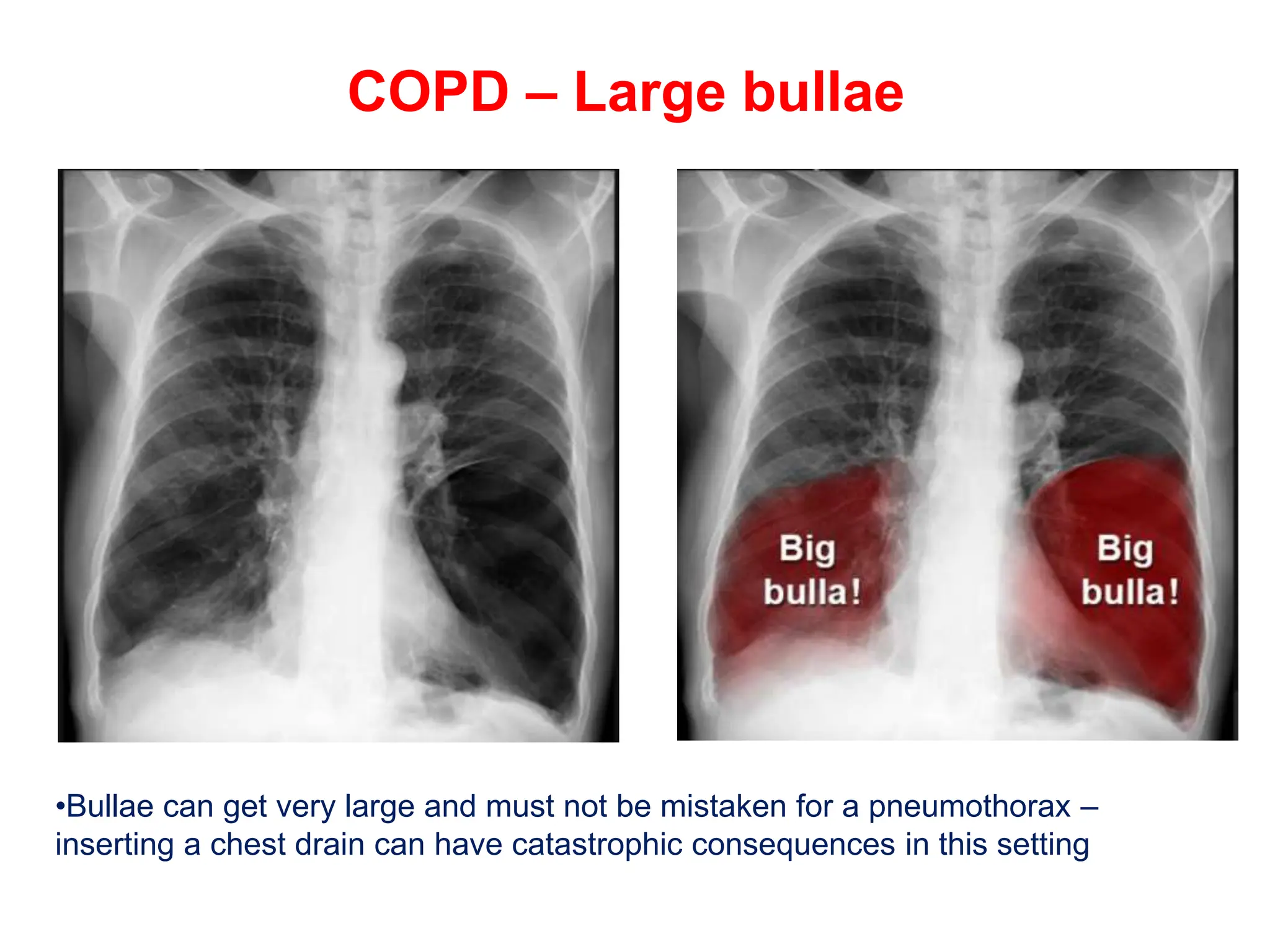
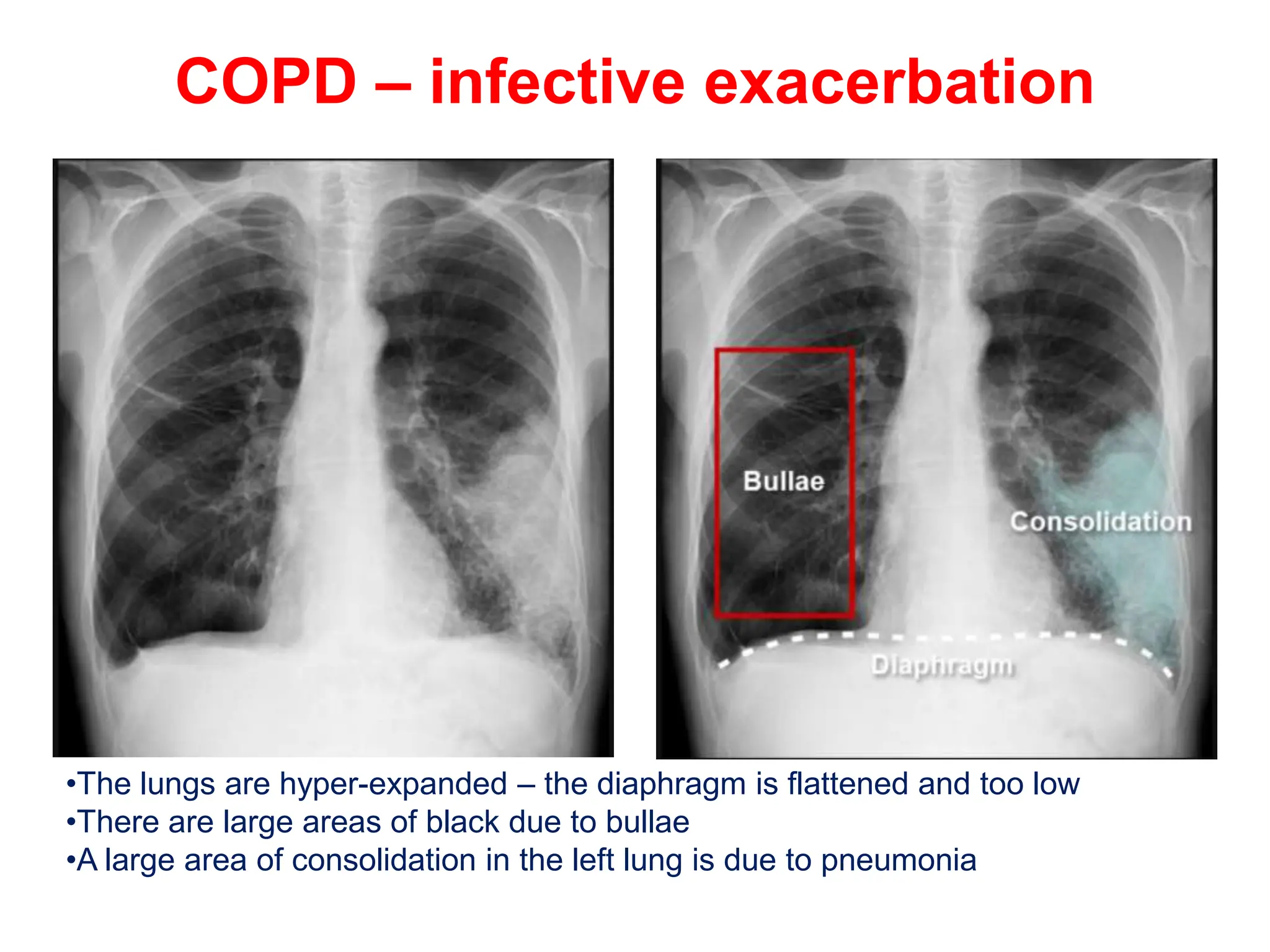
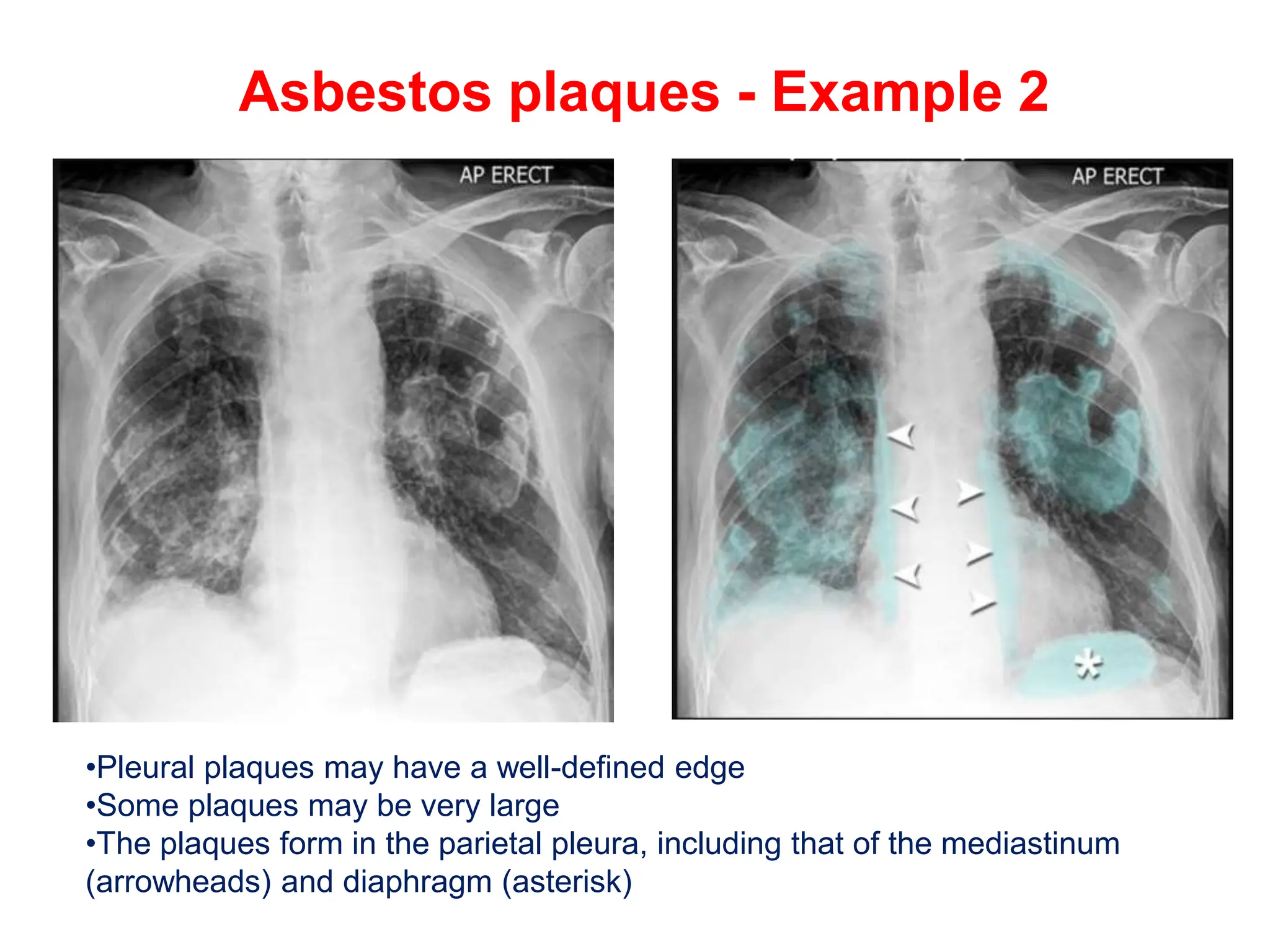
The document discusses various types of lung consolidations, their radiological features, and associated conditions as seen in chest X-rays. It covers examples including pneumonia, tuberculosis, lung contusions, and emphysema, identifying specific signs like air bronchograms and pathological changes. Additionally, it mentions the presence of lung cavities, fibrosis, and asbestos-related conditions, emphasizing their diagnostic implications.