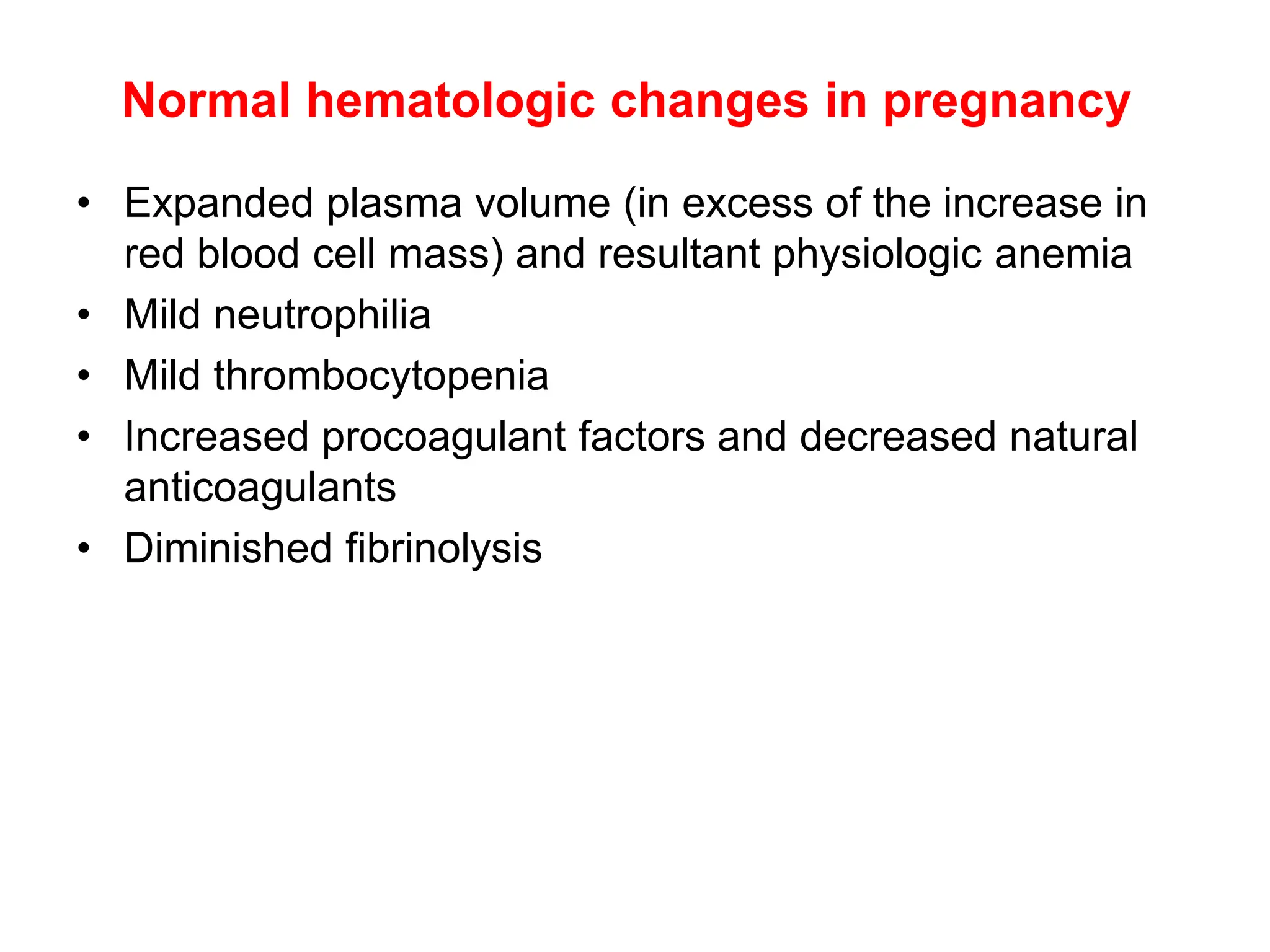
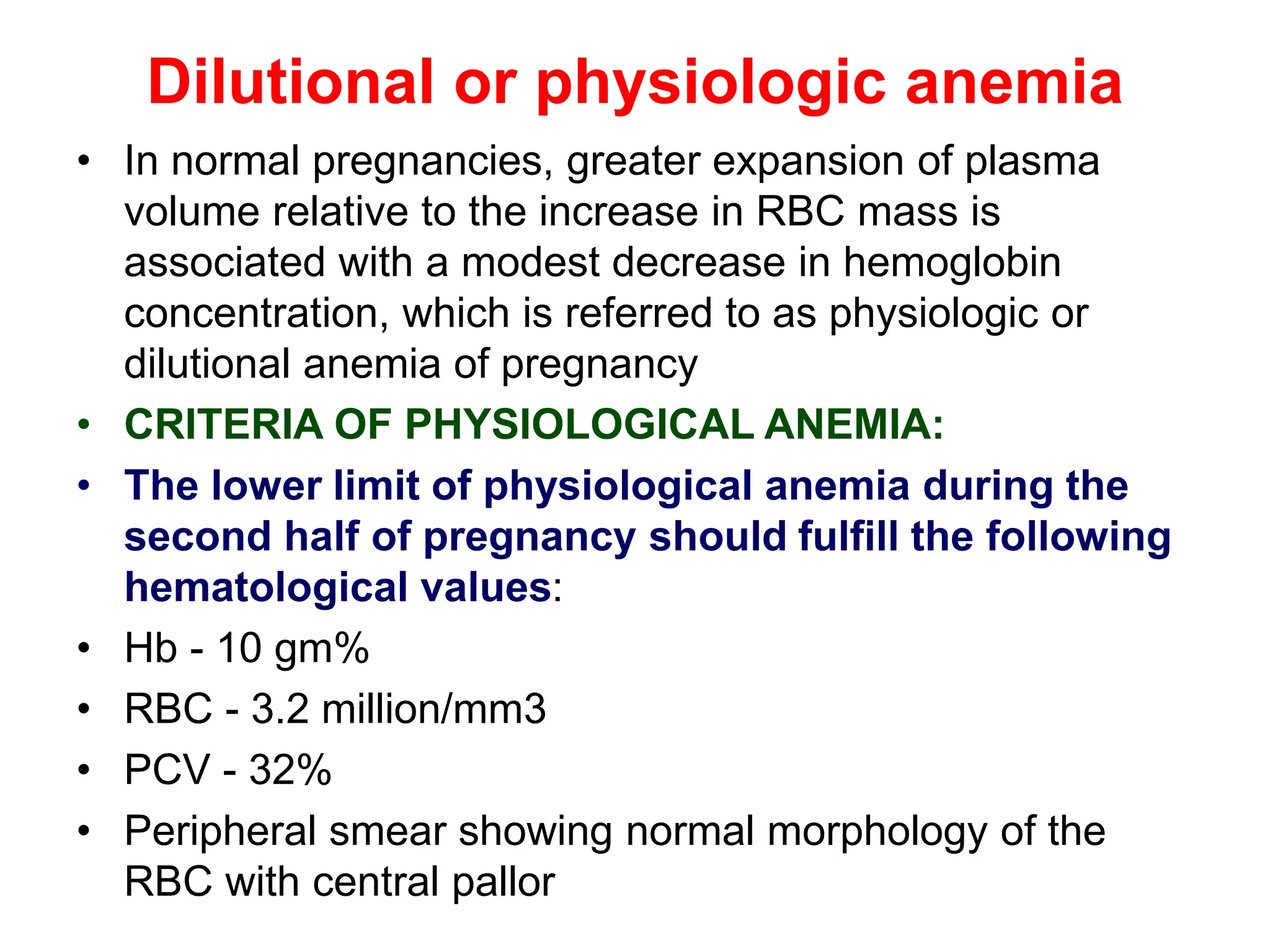
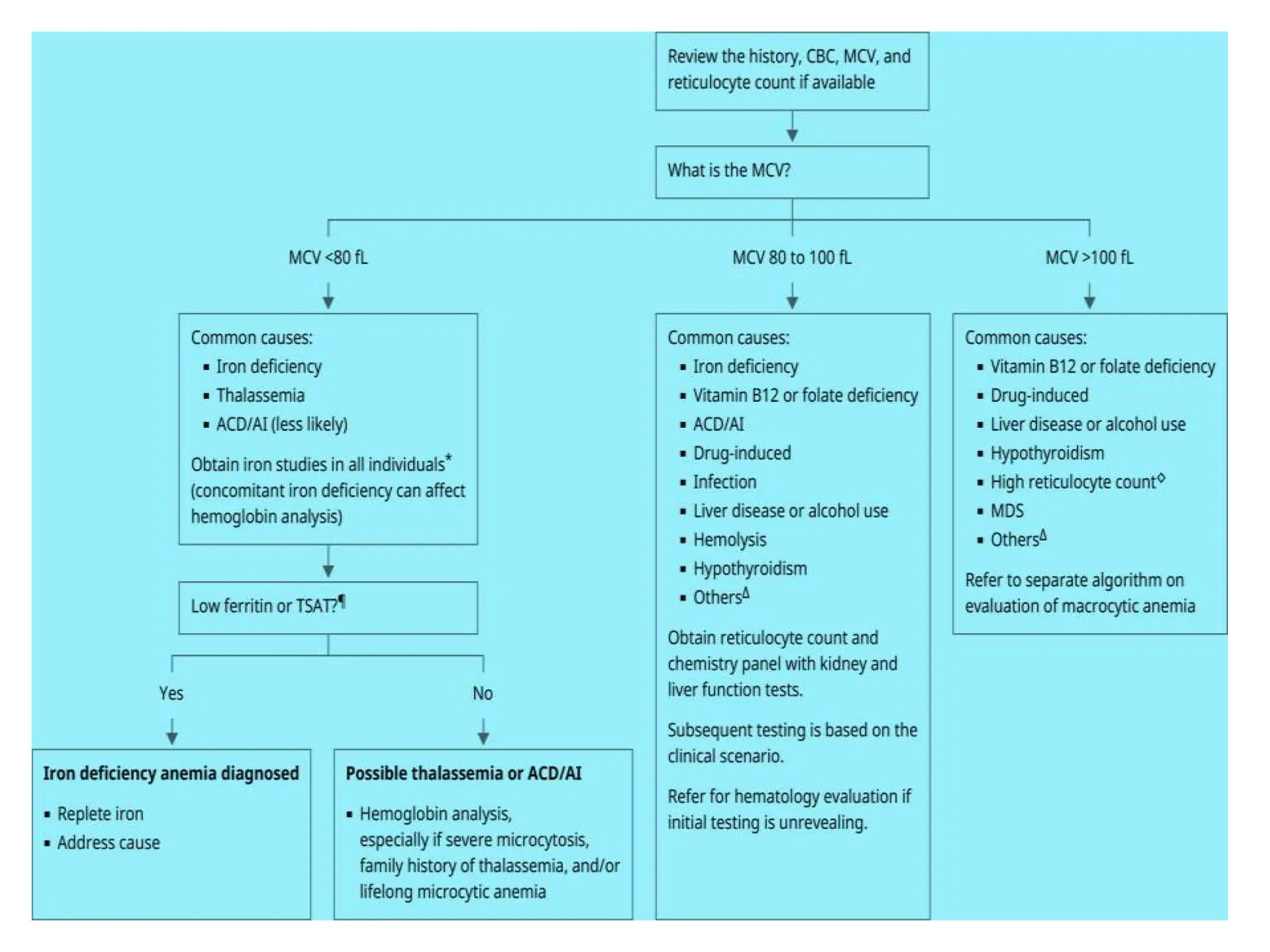
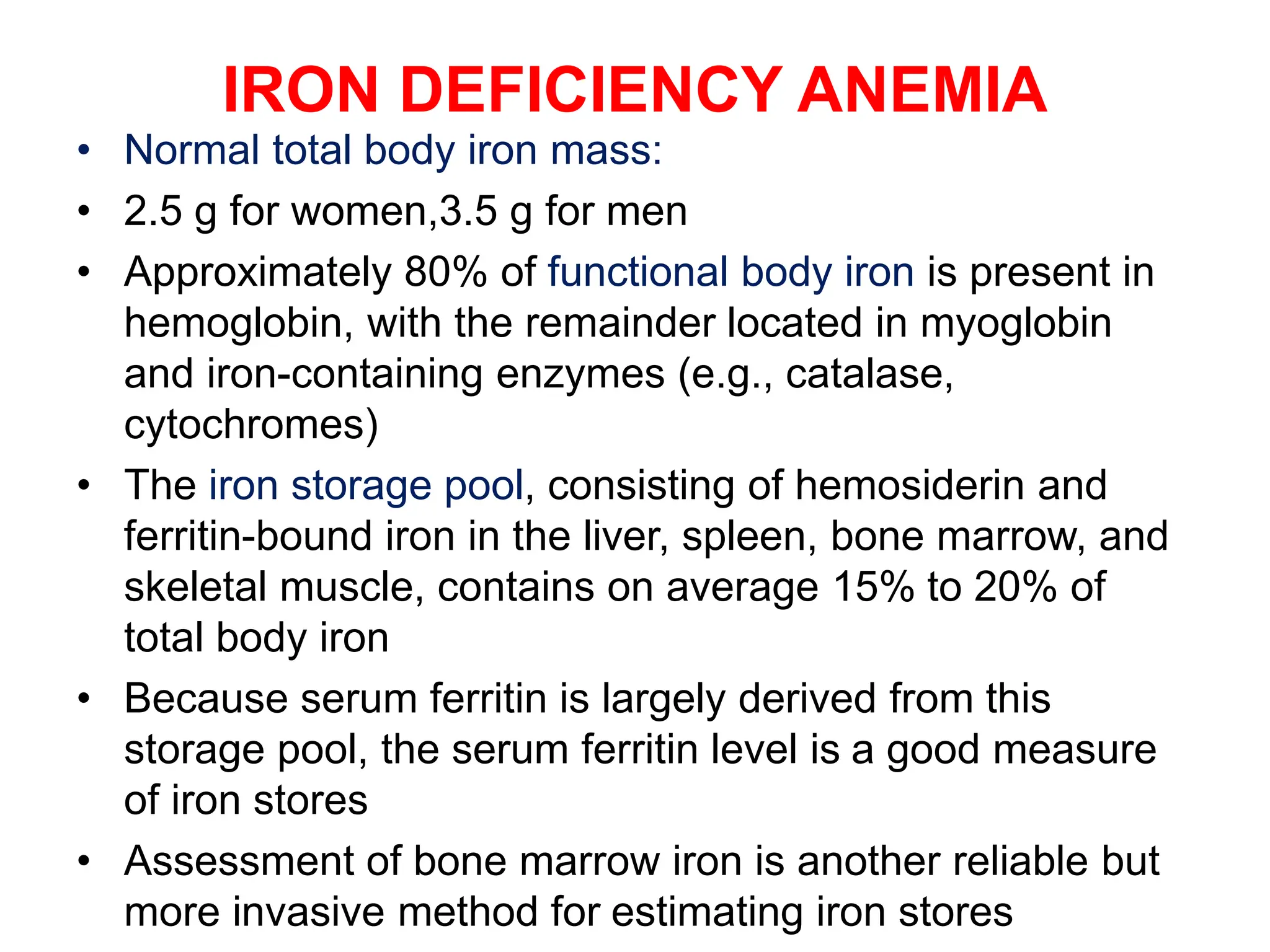
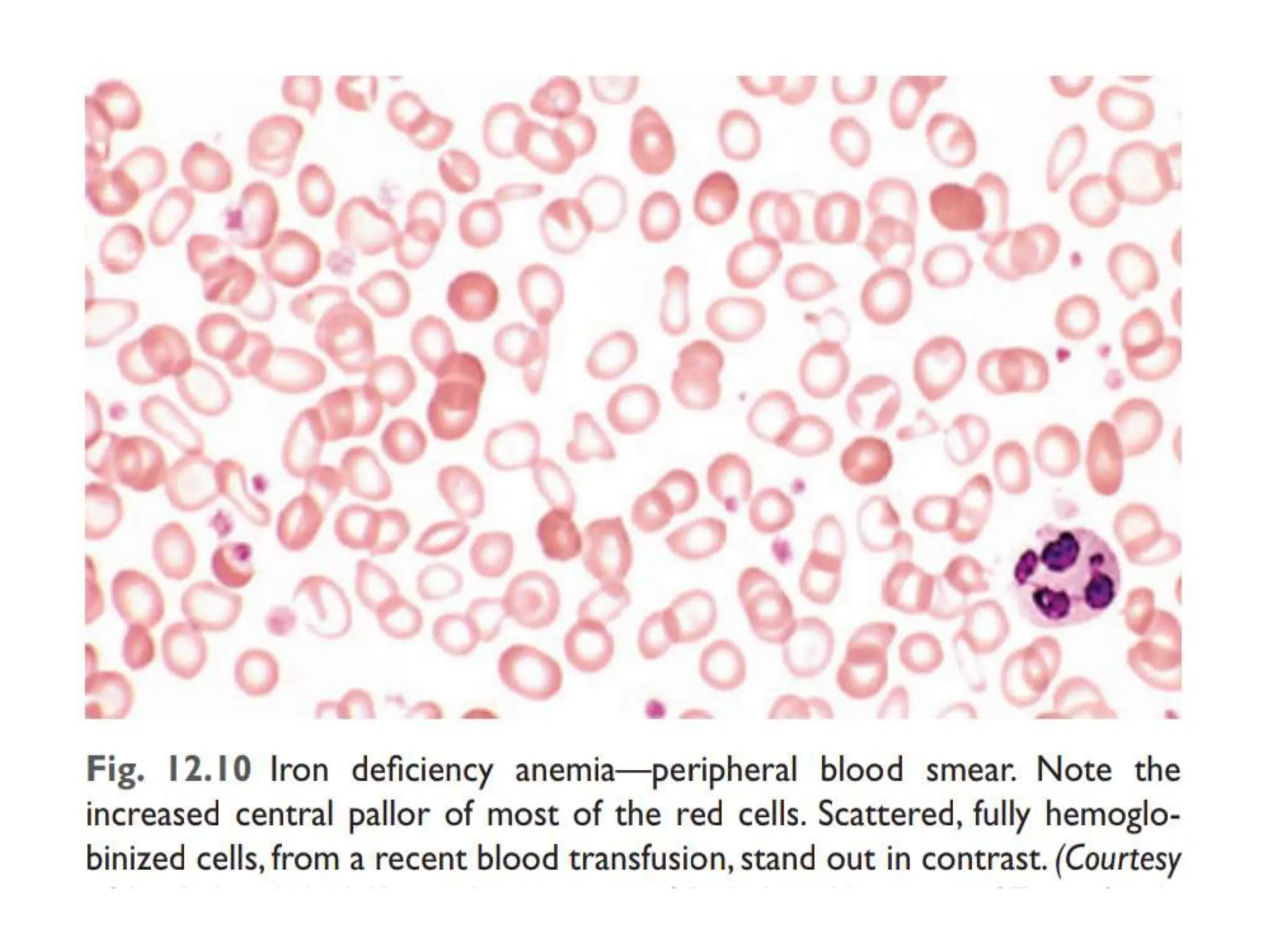
The document discusses anemia in pregnancy, specifically iron deficiency anemia, defining it as a reduction in hemoglobin levels below 10 g/dl during pregnancy. It covers classifications, physiological versus pathological anemia, causes, diagnosis, complications, and treatment options, emphasizing the importance of iron supplementation and dietary intake for prevention. Additionally, it highlights the risks associated with anemia during pregnancy for both the mother and baby, along with the recommended therapeutic approaches.