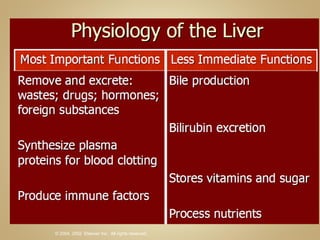
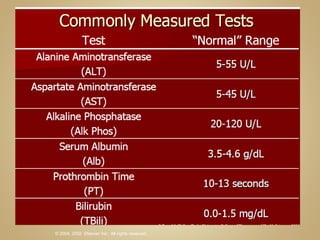
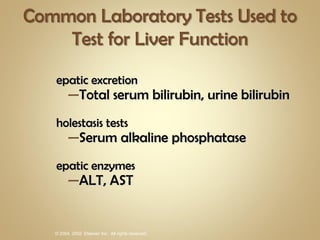
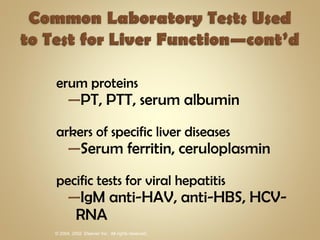
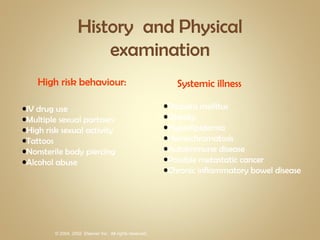
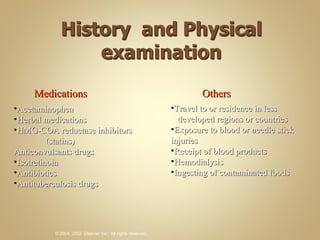
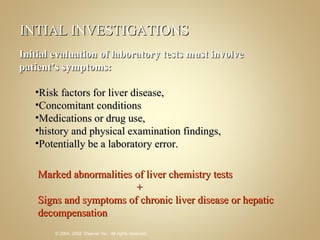
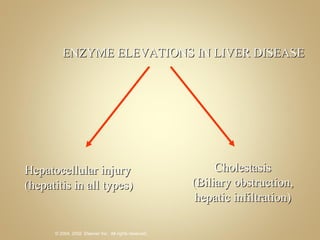
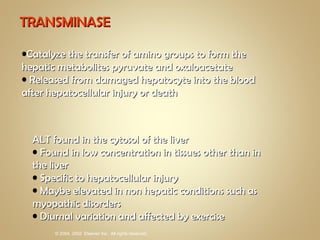
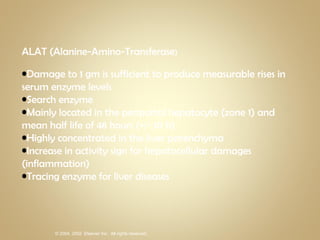
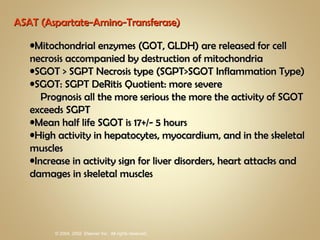
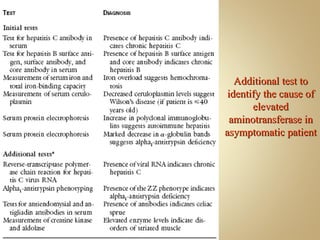
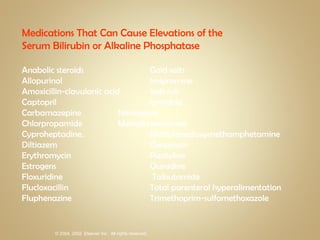
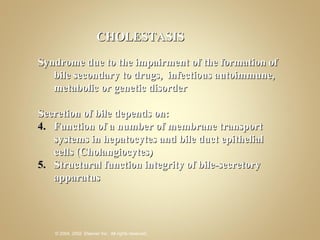
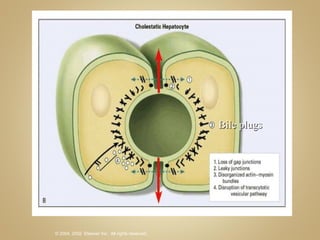
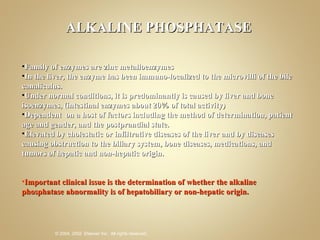
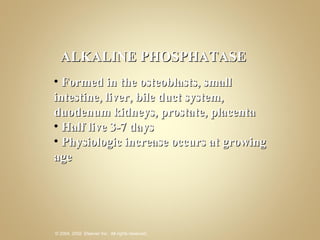
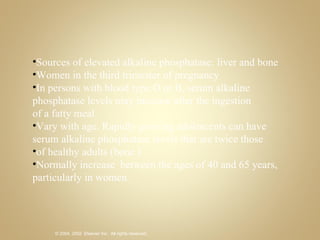
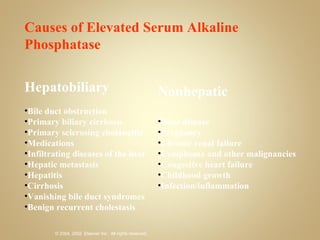
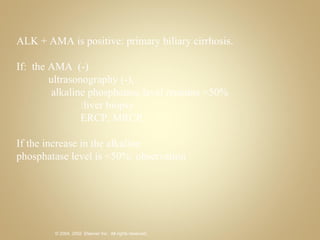
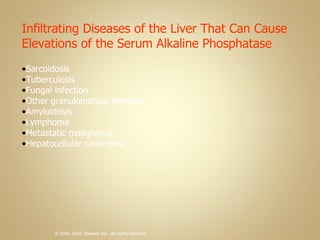
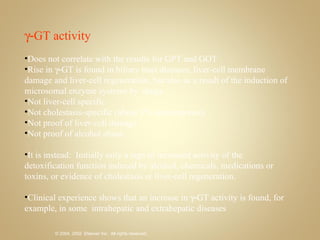
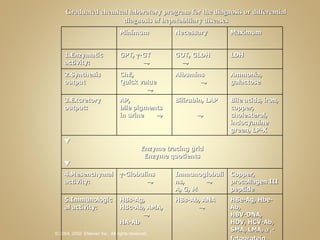
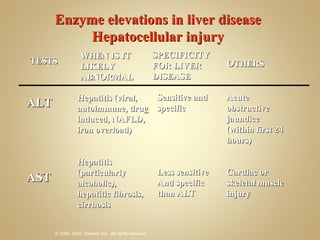
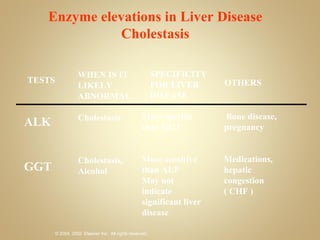
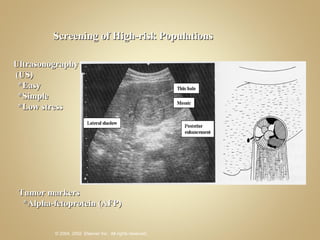
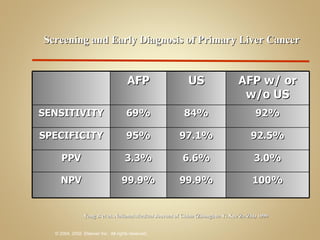
The document discusses various laboratory tests used to evaluate liver function and disease. It describes tests for hepatocellular damage like ALT and AST, tests for cholestasis like alkaline phosphatase, and tests for liver synthetic function like albumin. Common causes of abnormal liver enzymes are also summarized, along with risk factors for liver disease.