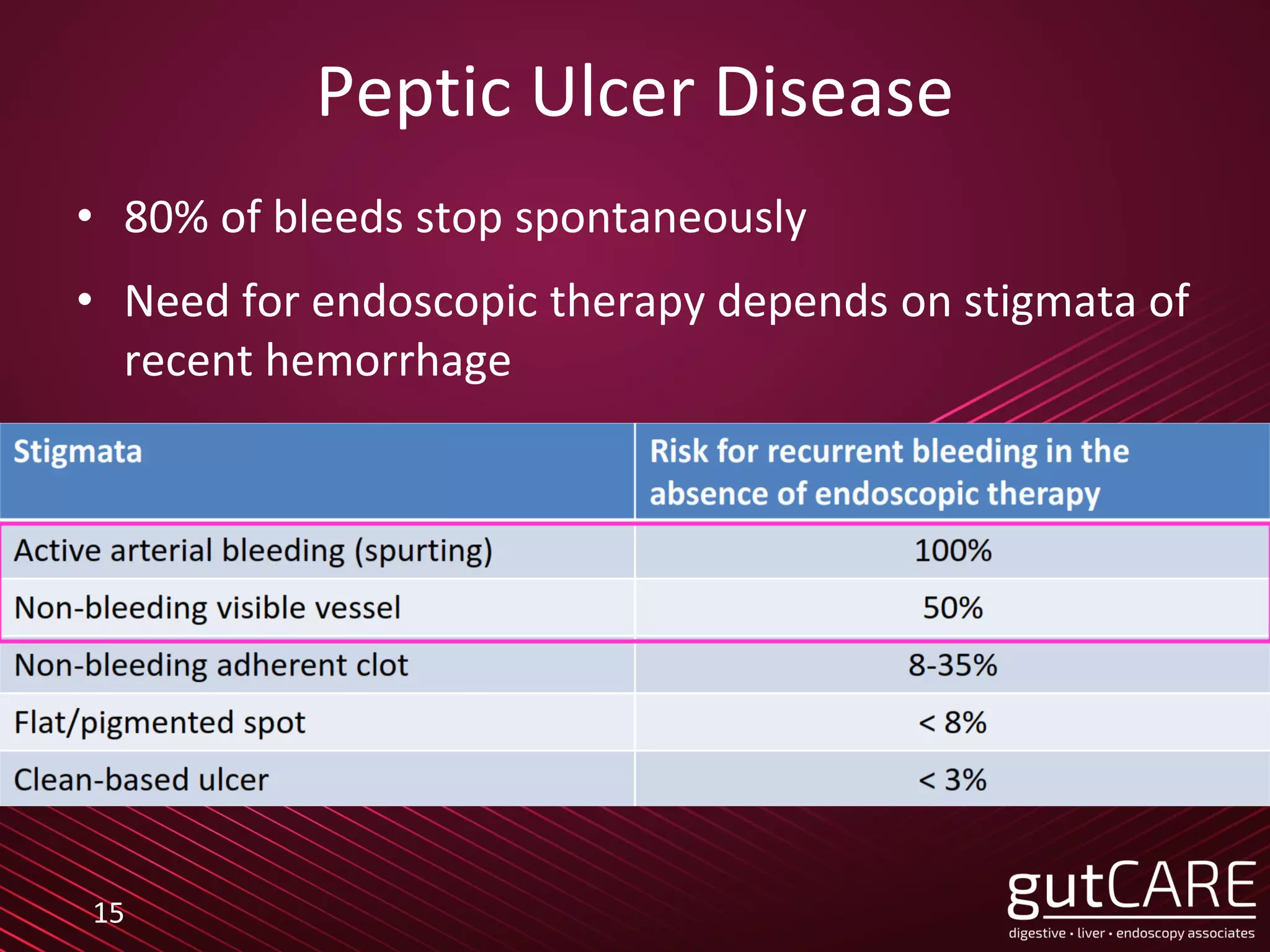
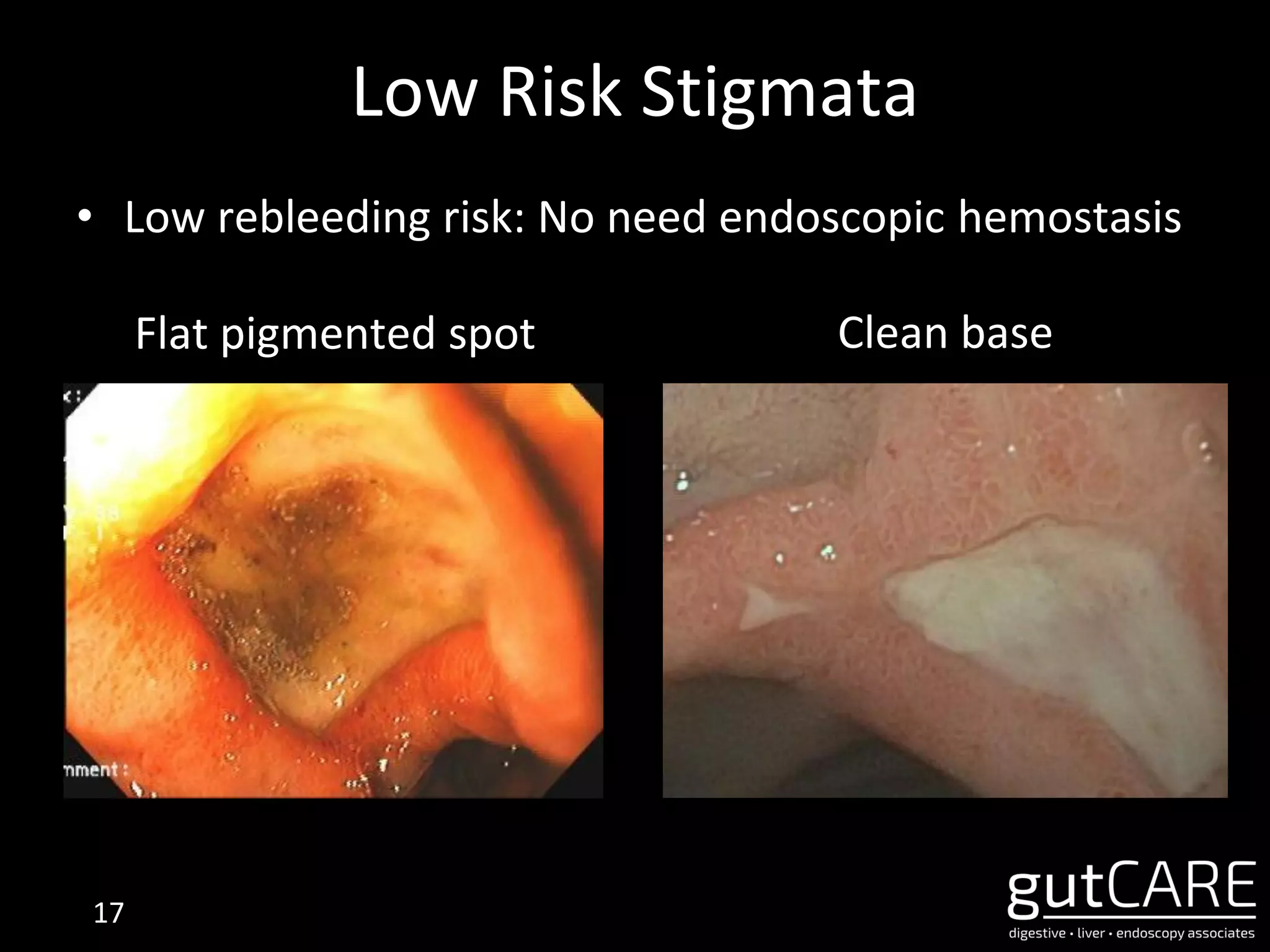
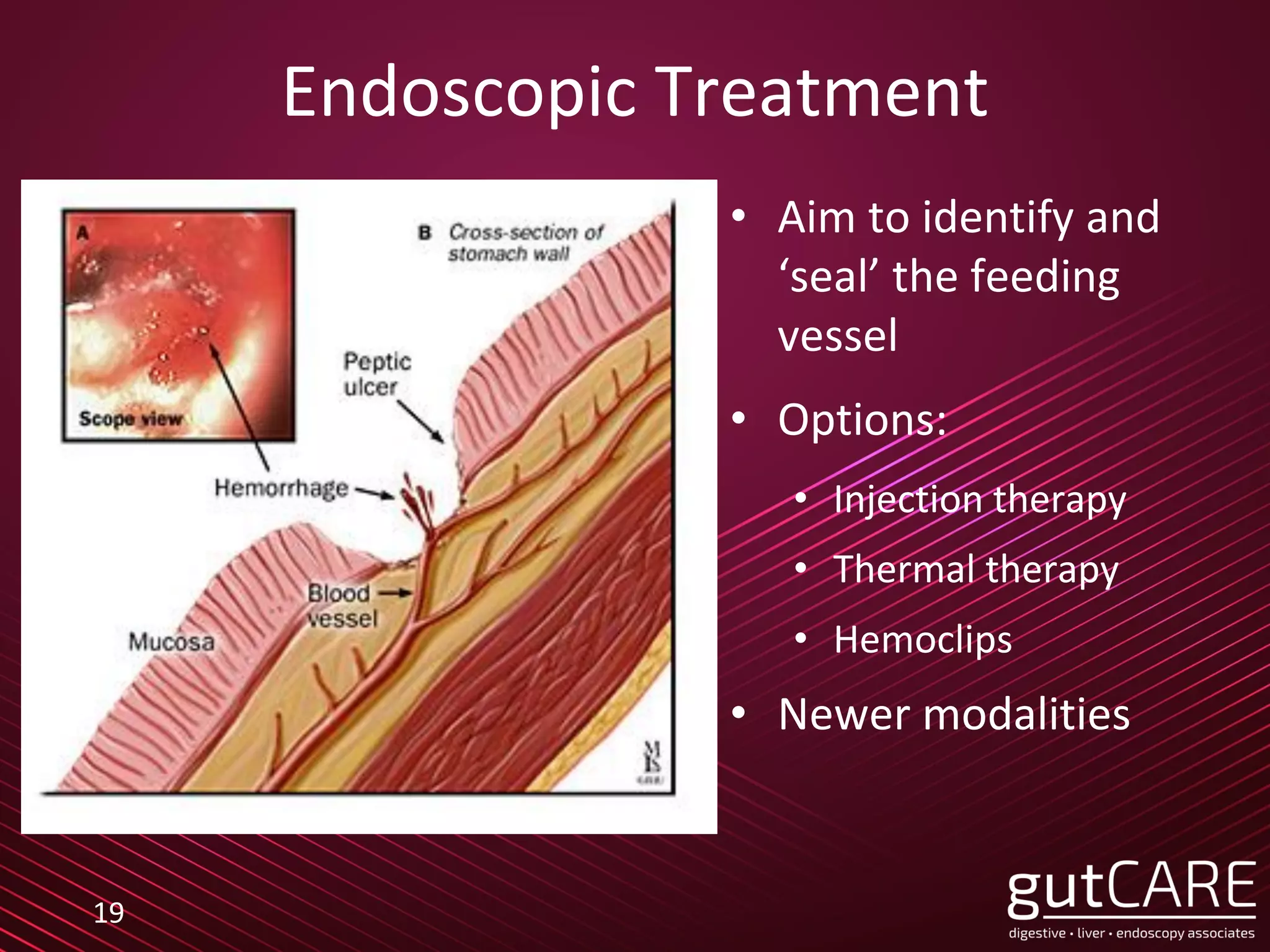
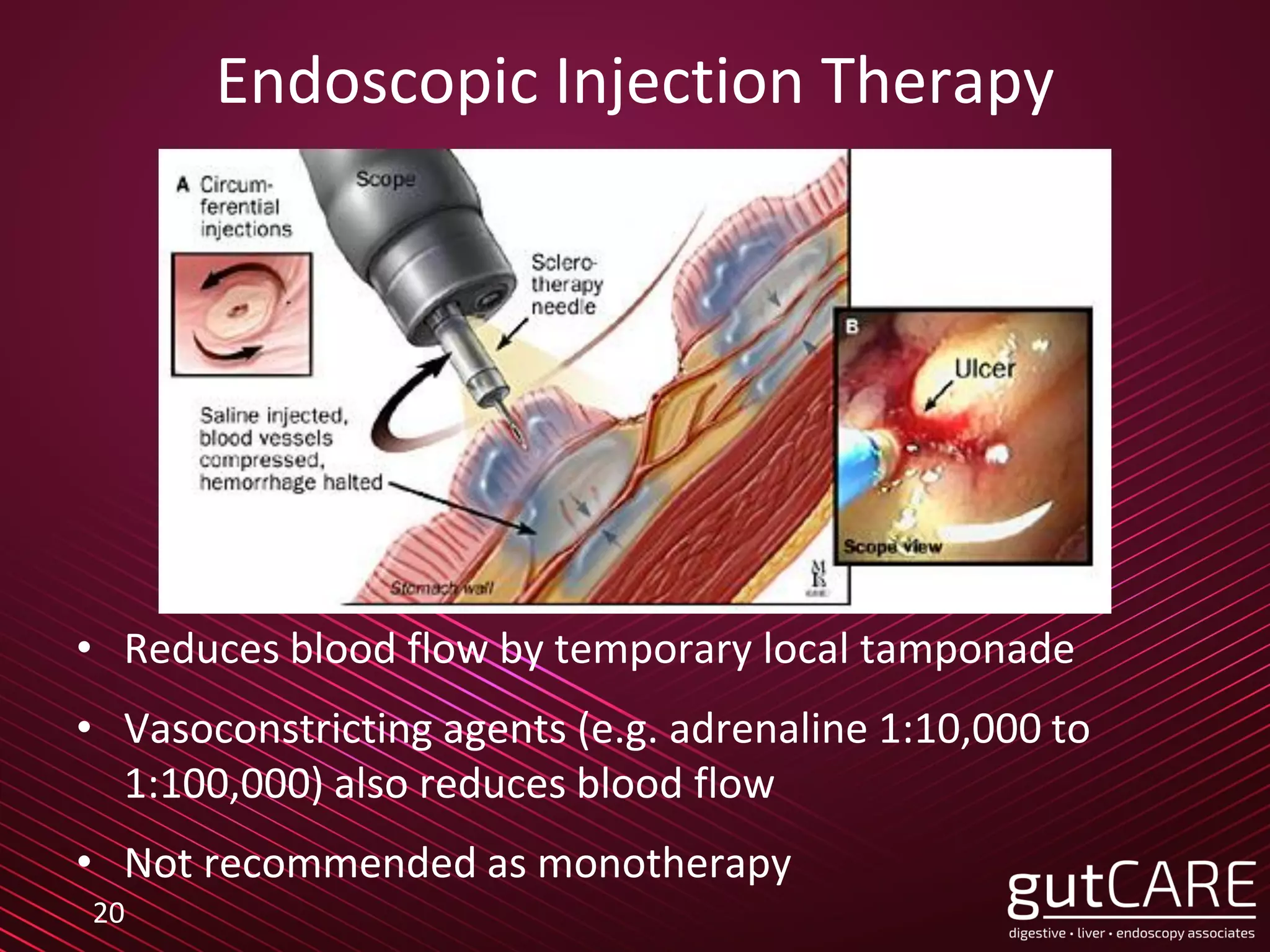
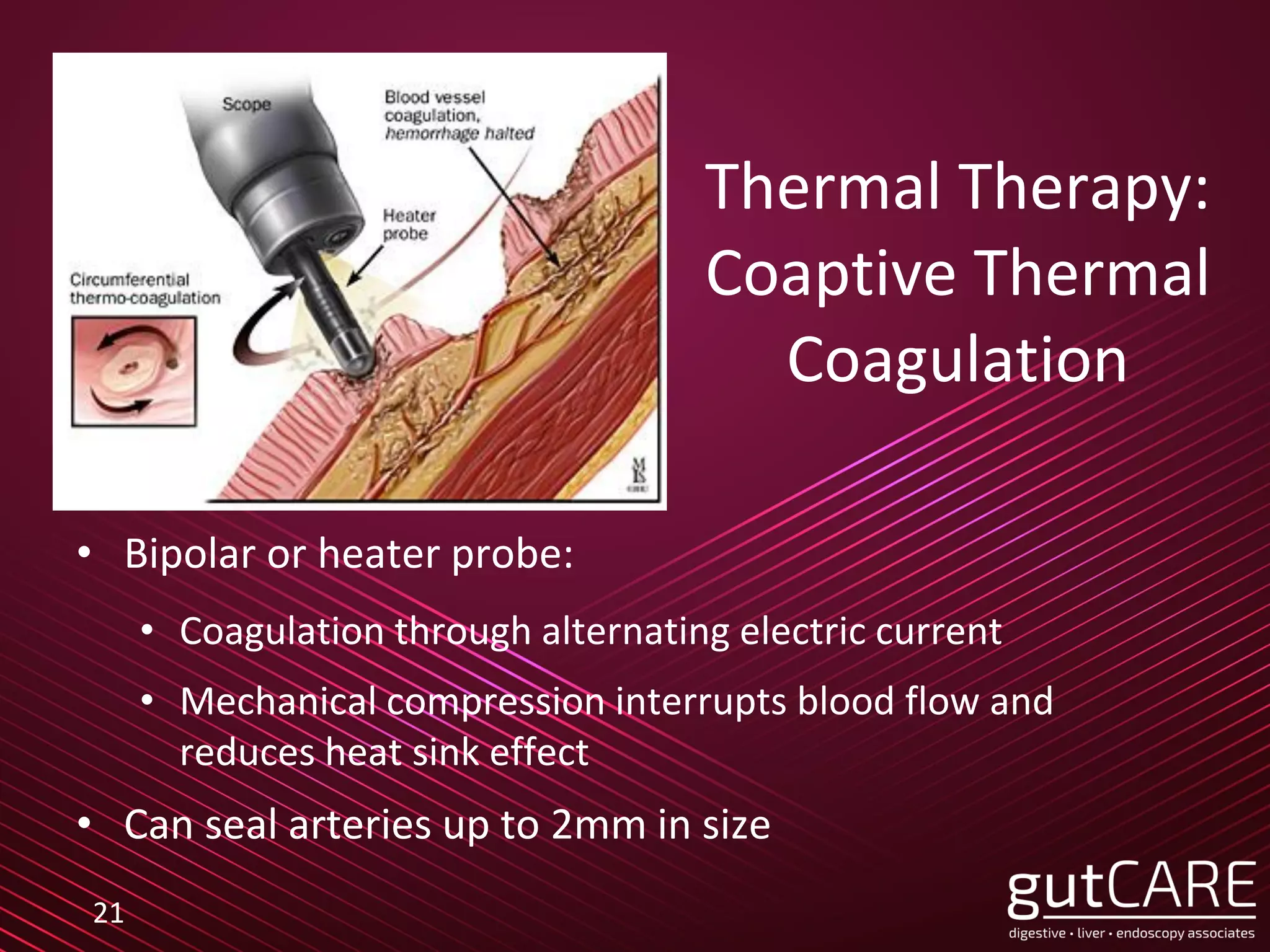
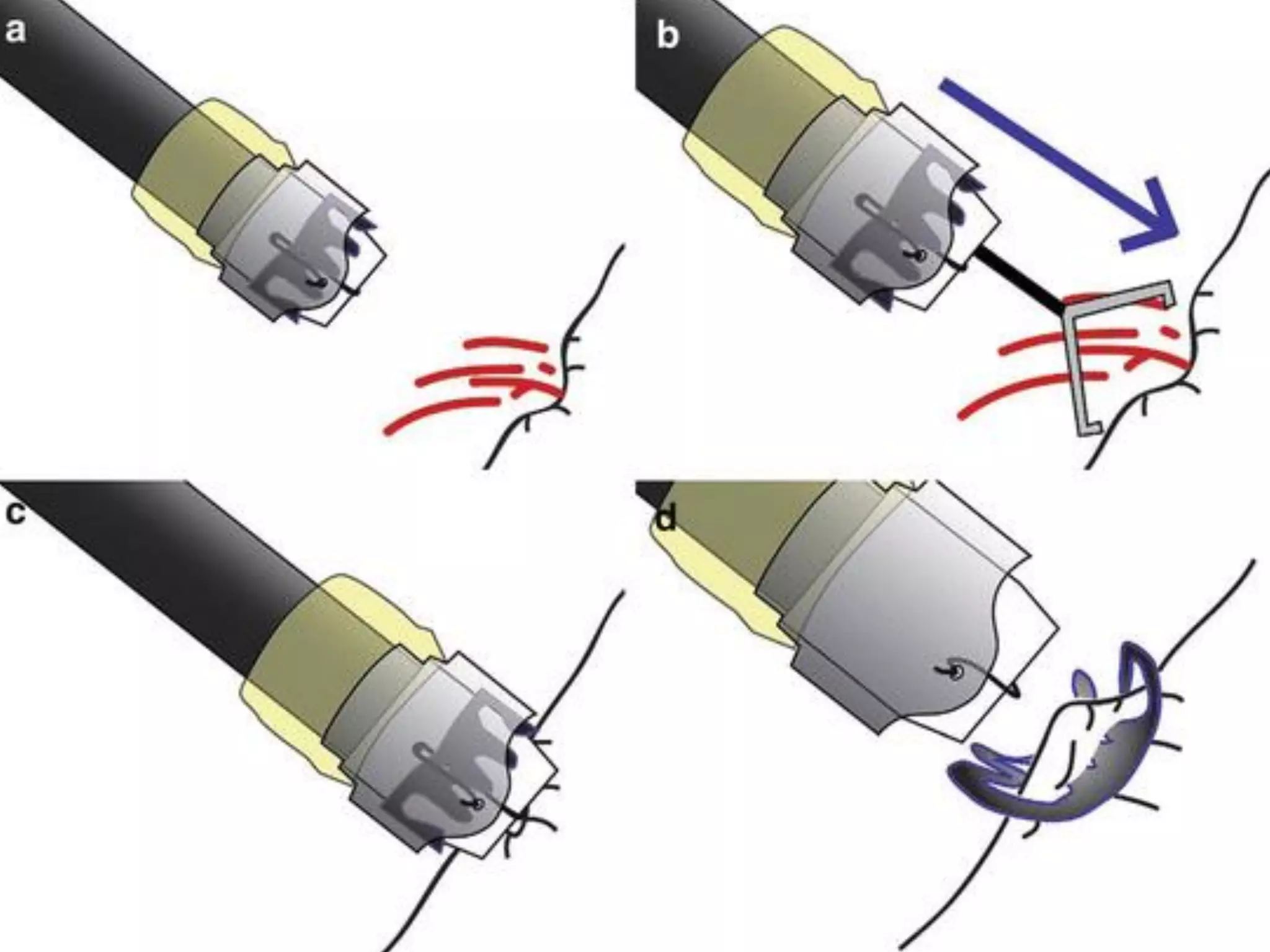
The lecture by Dr. Jarrod Lee focuses on endoscopic hemostasis for gastrointestinal bleeding, detailing management strategies for upper and lower GI bleeds, including peptic ulcer disease and variceal bleeding. Key findings from studies emphasize the benefits of restrictive transfusion strategies and early endoscopic intervention. Various endoscopic techniques and modalities are outlined, highlighting the importance of tailored approaches based on the bleeding source and patient condition.