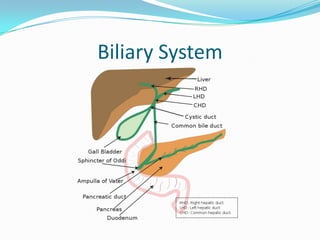
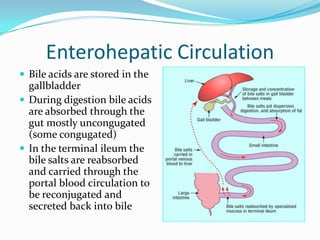
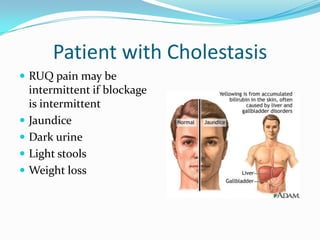
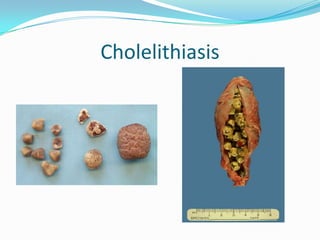
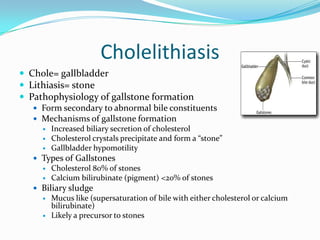
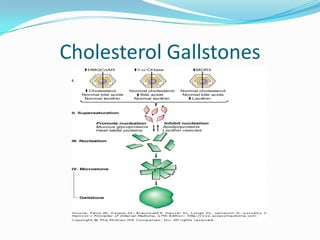
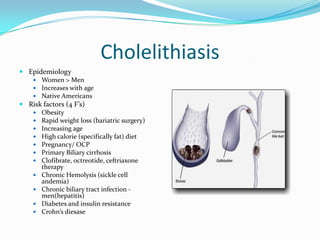
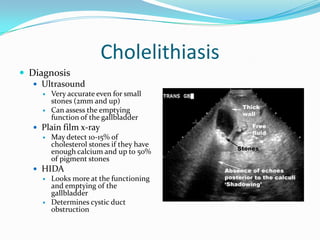
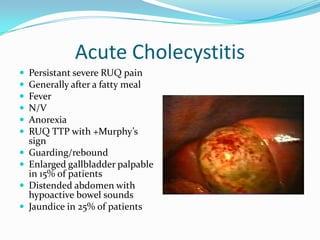
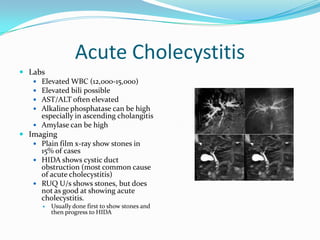
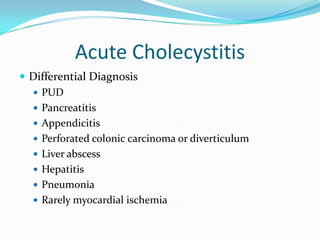
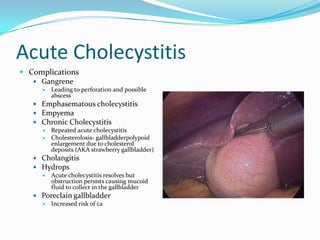
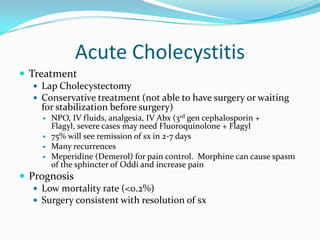
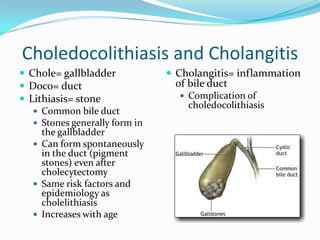
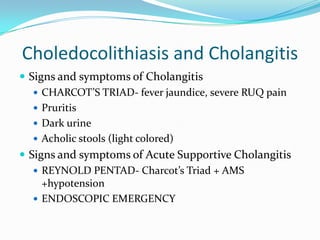
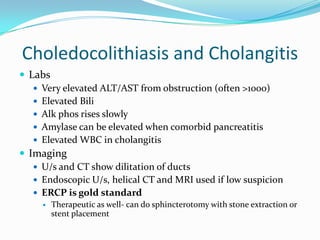
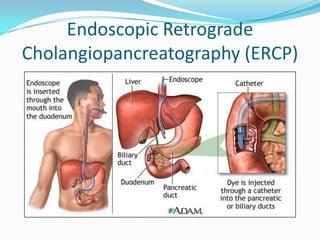
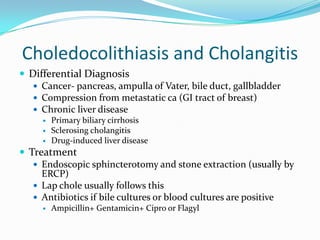
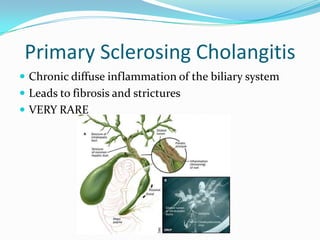
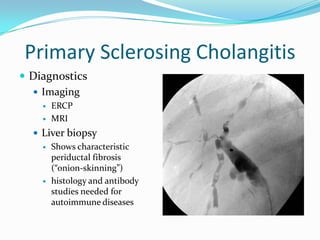
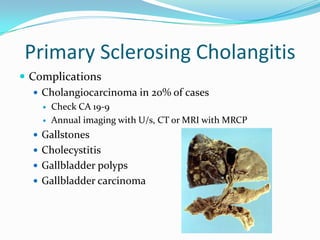
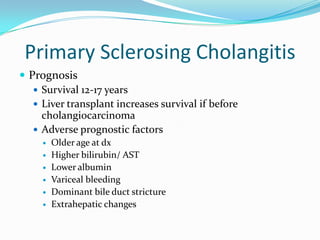
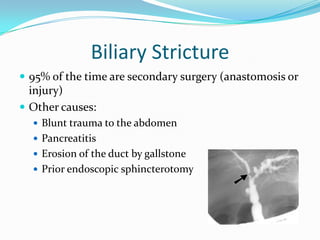
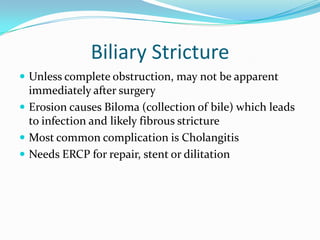
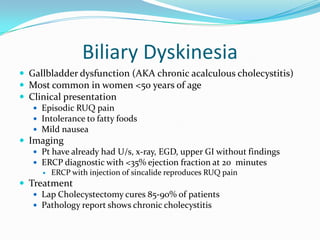
This document defines various components of the biliary system including bile, bile salts, and bile acids. It describes bile acid metabolism and the enterohepatic circulation. It discusses cholestasis, approaches to diagnosing a patient with cholestasis, and various causes of cholestasis including gallstones. It describes the pathophysiology, risk factors, clinical features, diagnosis, and treatment of gallstone disease. It also discusses other biliary diseases and conditions such as primary sclerosing cholangitis, biliary strictures, and biliary dyskinesia.