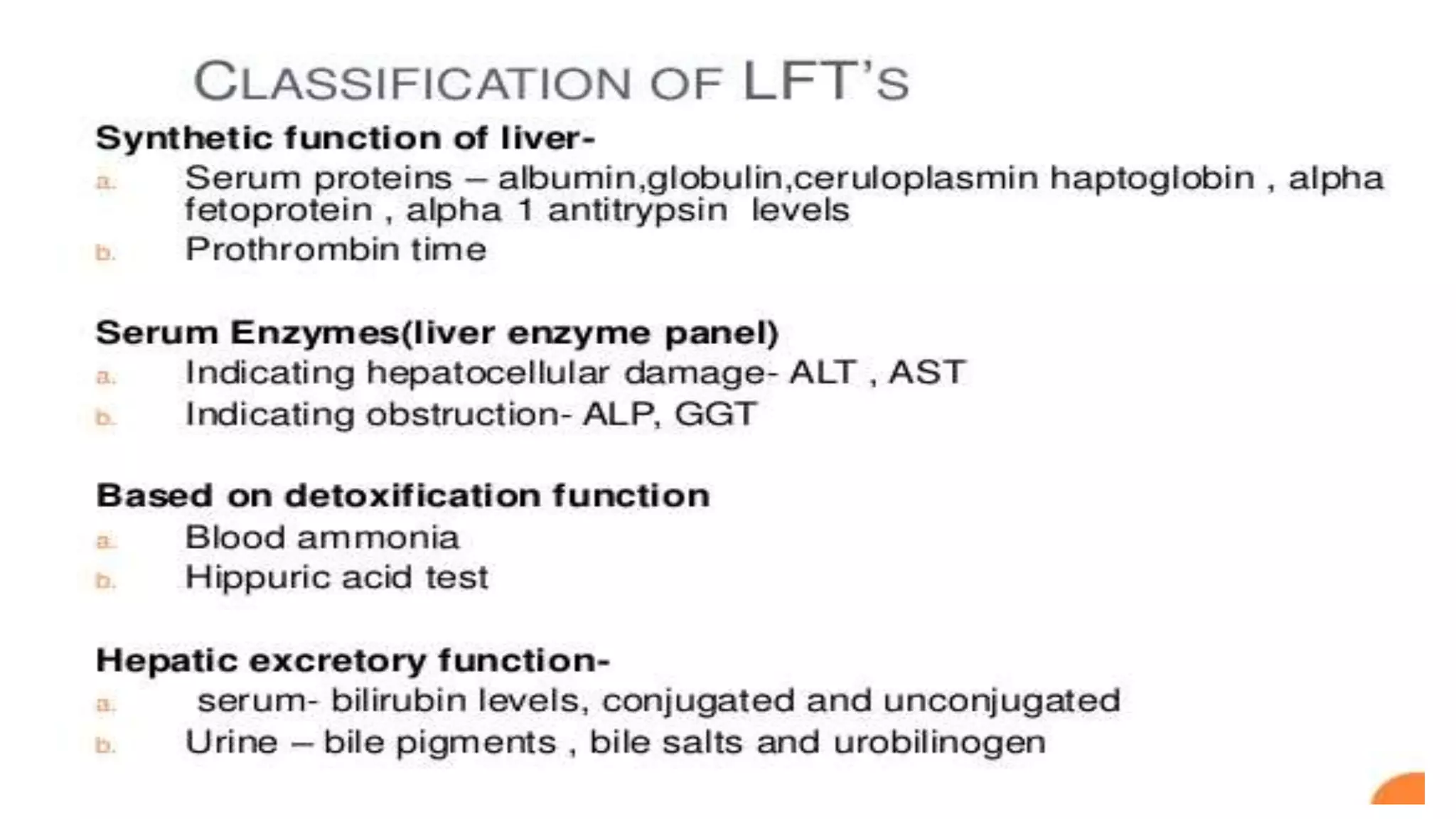
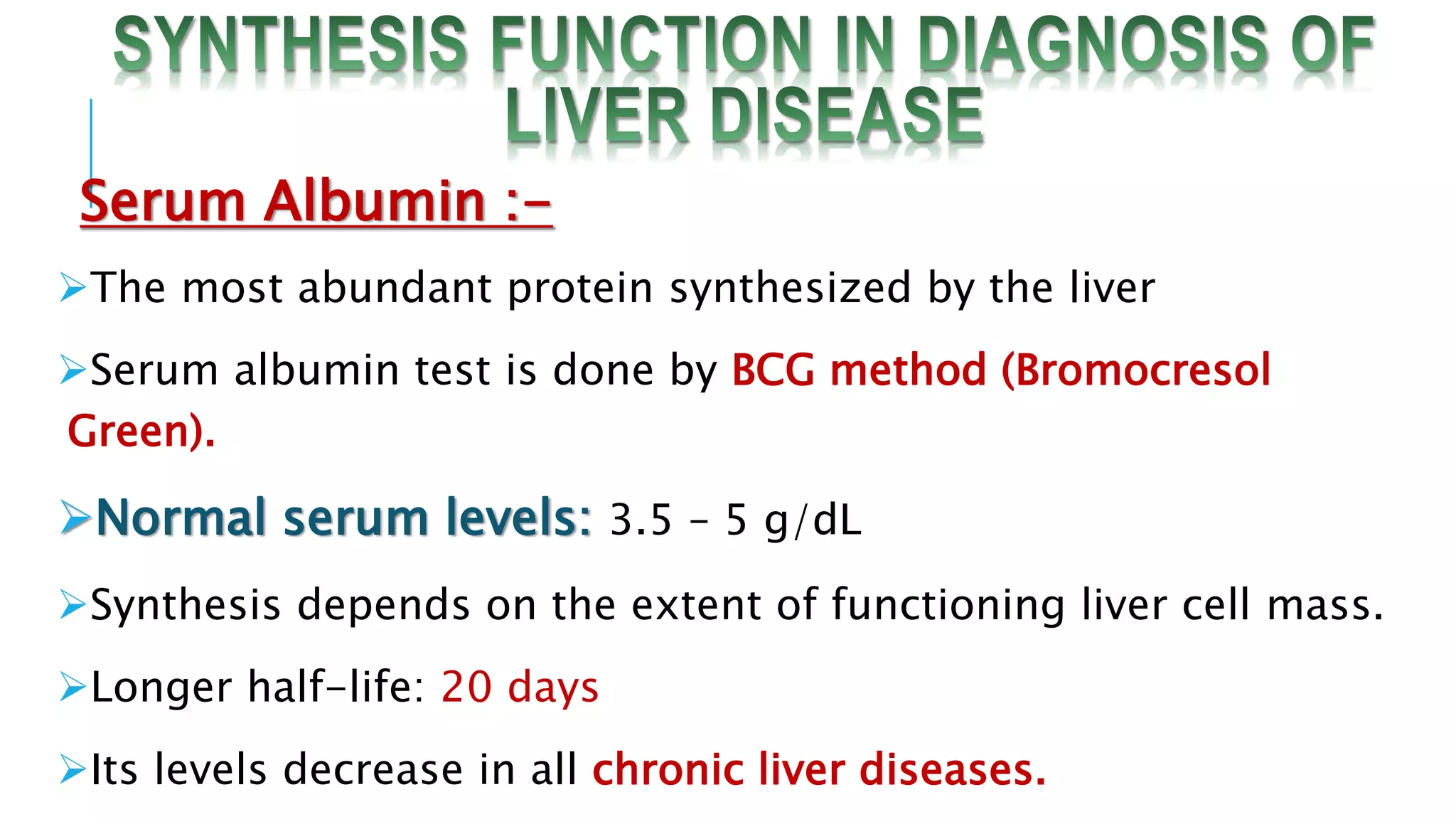
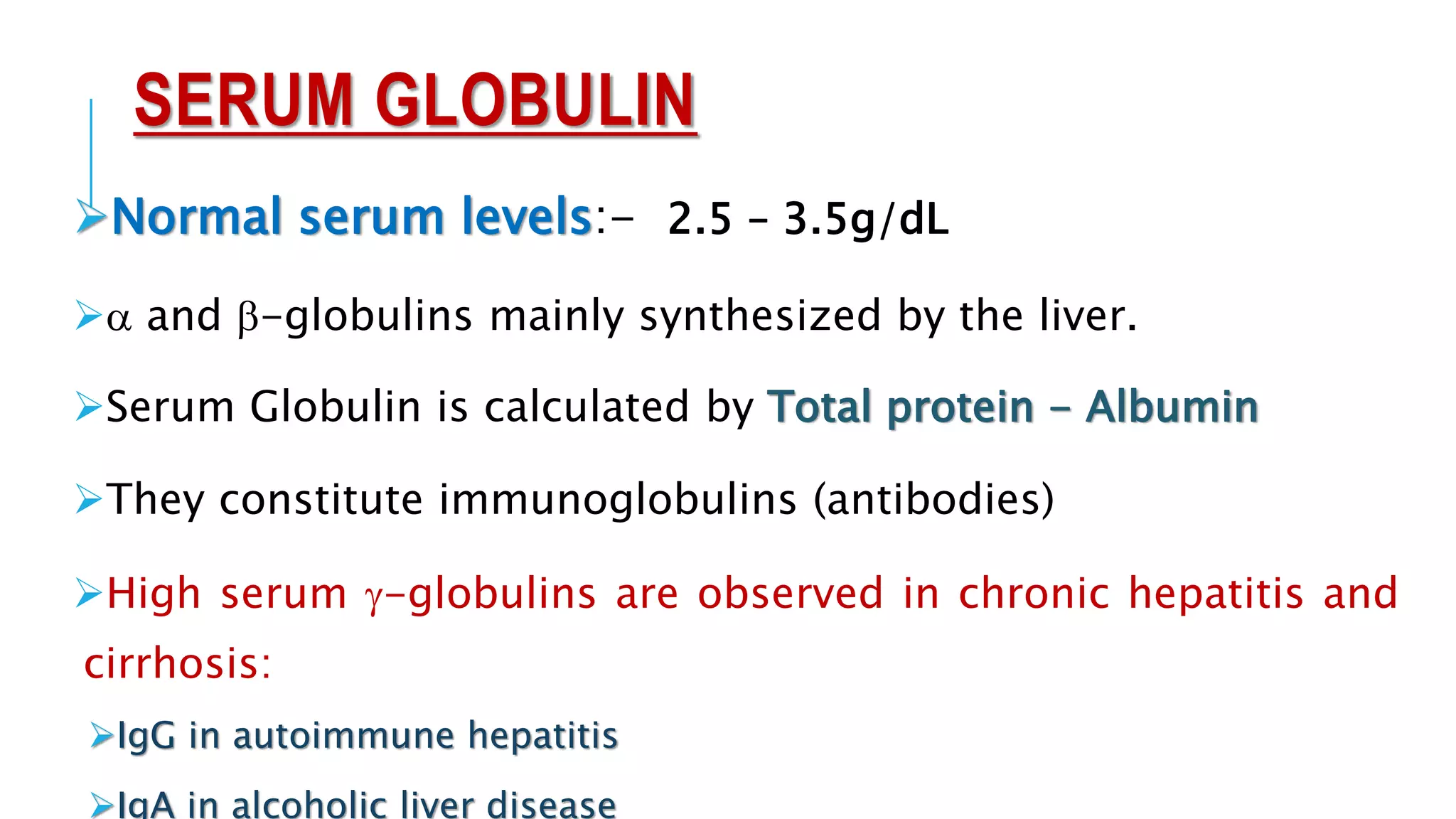
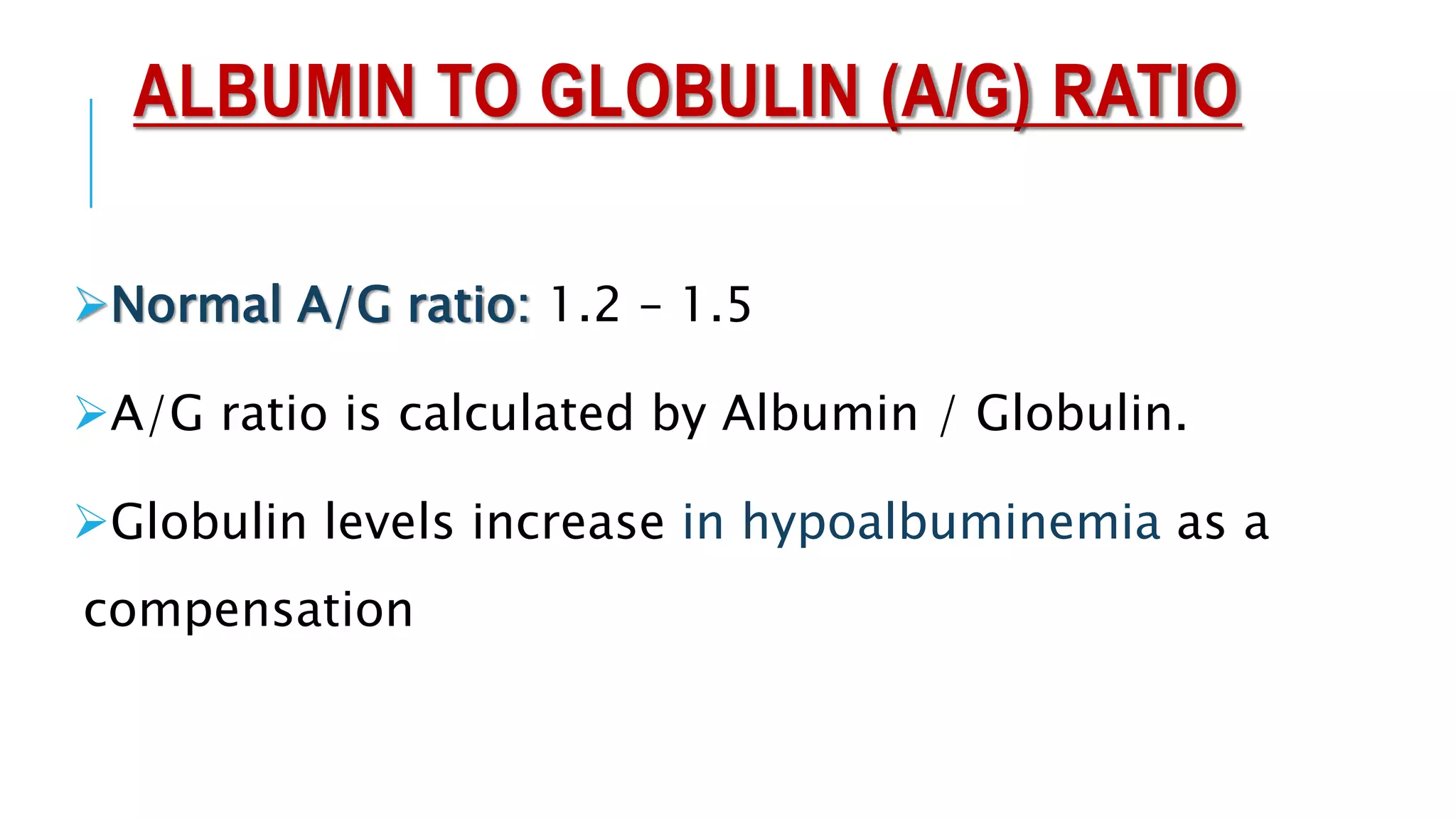
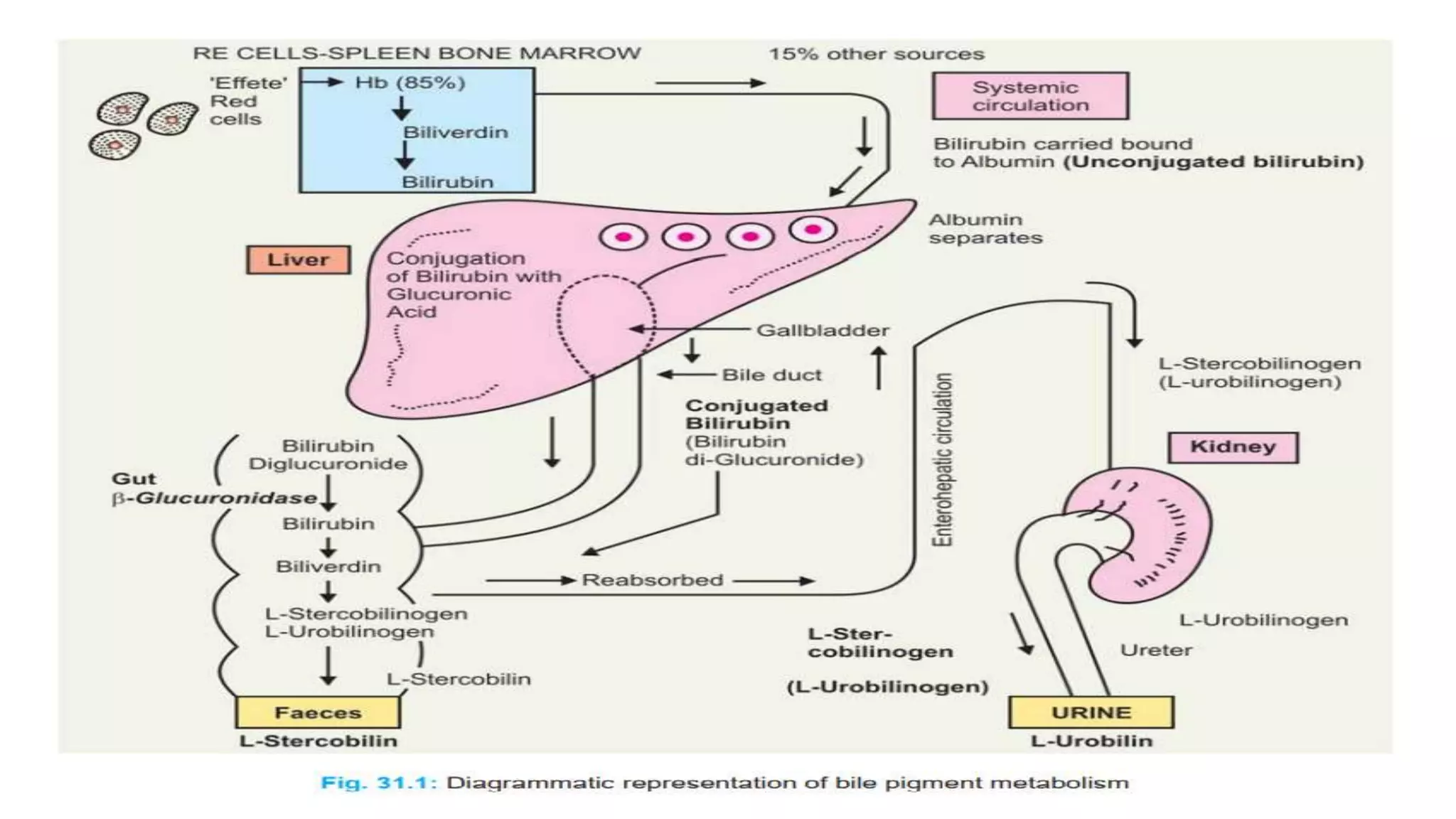
Liver function tests (LFTs) are biochemical blood tests that are useful for detecting and monitoring liver diseases. Common LFTs examine levels of serum albumin, globulin, bilirubin, and liver enzymes. Elevated levels of certain enzymes like ALT and AST indicate liver cell damage, while increased alkaline phosphatase or globulins may point to obstruction or inflammation. Together, LFT results can help diagnose liver problems, distinguish between disease types, and gauge treatment effectiveness. LFTs are among the most frequently performed medical lab tests.