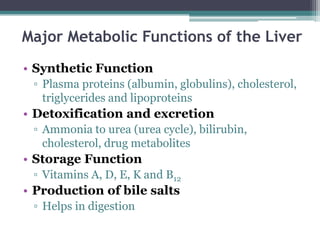
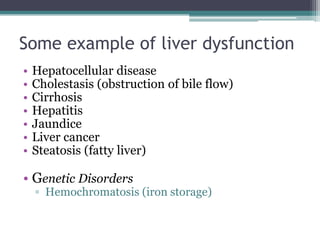
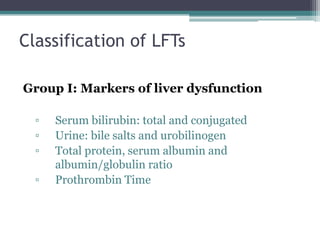
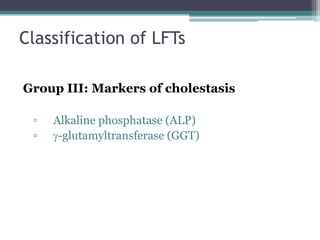
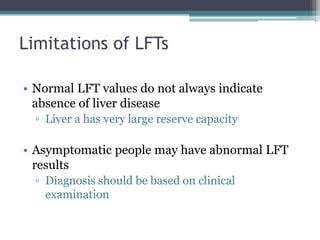
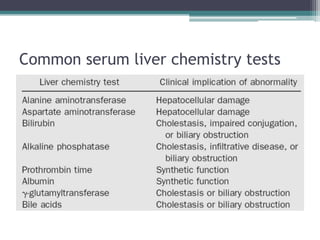
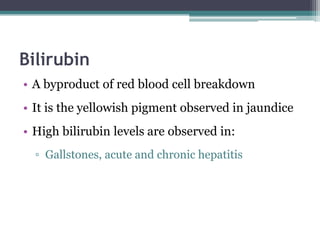
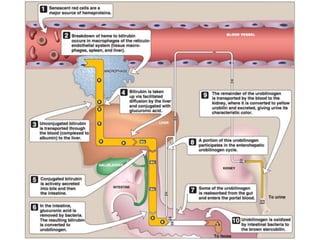
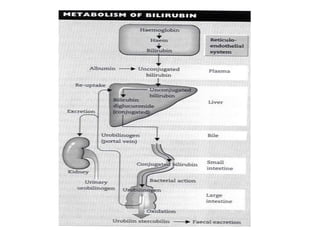
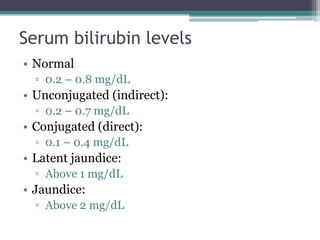
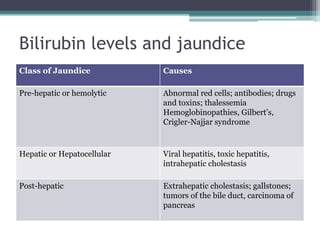
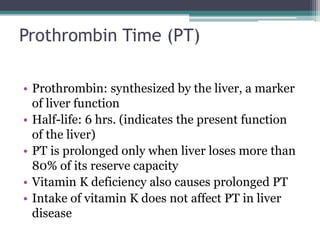
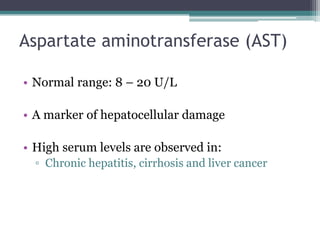
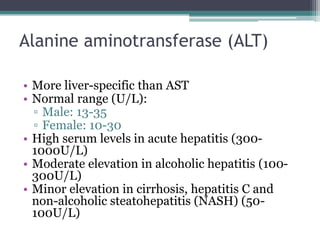
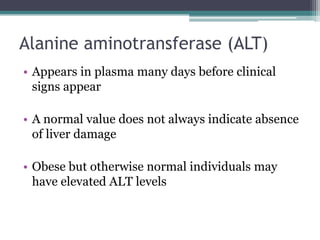
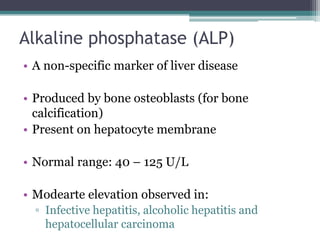
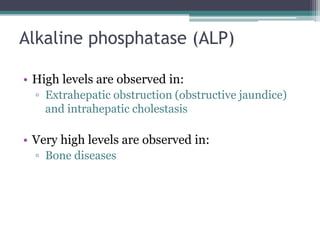
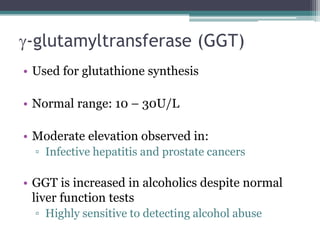
The document discusses liver function tests (LFTs), which are used to screen for and diagnose liver dysfunction. It outlines the major metabolic functions of the liver, causes of liver disease, and various markers that can be measured in LFTs to detect hepatic injury and assess liver function. These include liver enzymes, bilirubin, albumin, prothrombin time, alkaline phosphatase, and gamma-glutamyltransferase. The document explains what each marker indicates and the typical ranges seen in different types of liver disease. LFTs have limitations but can help identify the general type of liver disorder and monitor disease severity and treatment response.