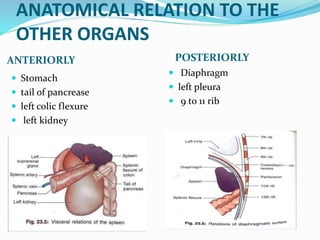
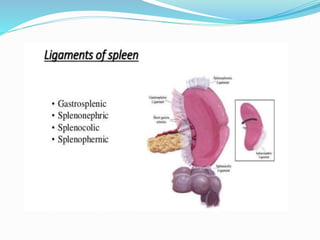
This document discusses the objectives, anatomy, indications for splenectomy, grading of splenic injuries, management options, postoperative care, and complications of splenectomy. The objectives include understanding the anatomy of the spleen, indications for splenectomy, splenectomy in trauma patients, grading and managing splenic injuries, postoperative care and complications, vaccination protocols, and educating asplenic patients. The anatomy, blood supply, drainage, and relations of the spleen are described. Indications, imaging, operative versus non-operative management, and surgical techniques including splenectomy, splenorrhaphy, and partial splenectomy are outlined. Postoperative care, early complications, late complications, deep vein thrombosis prophylaxis