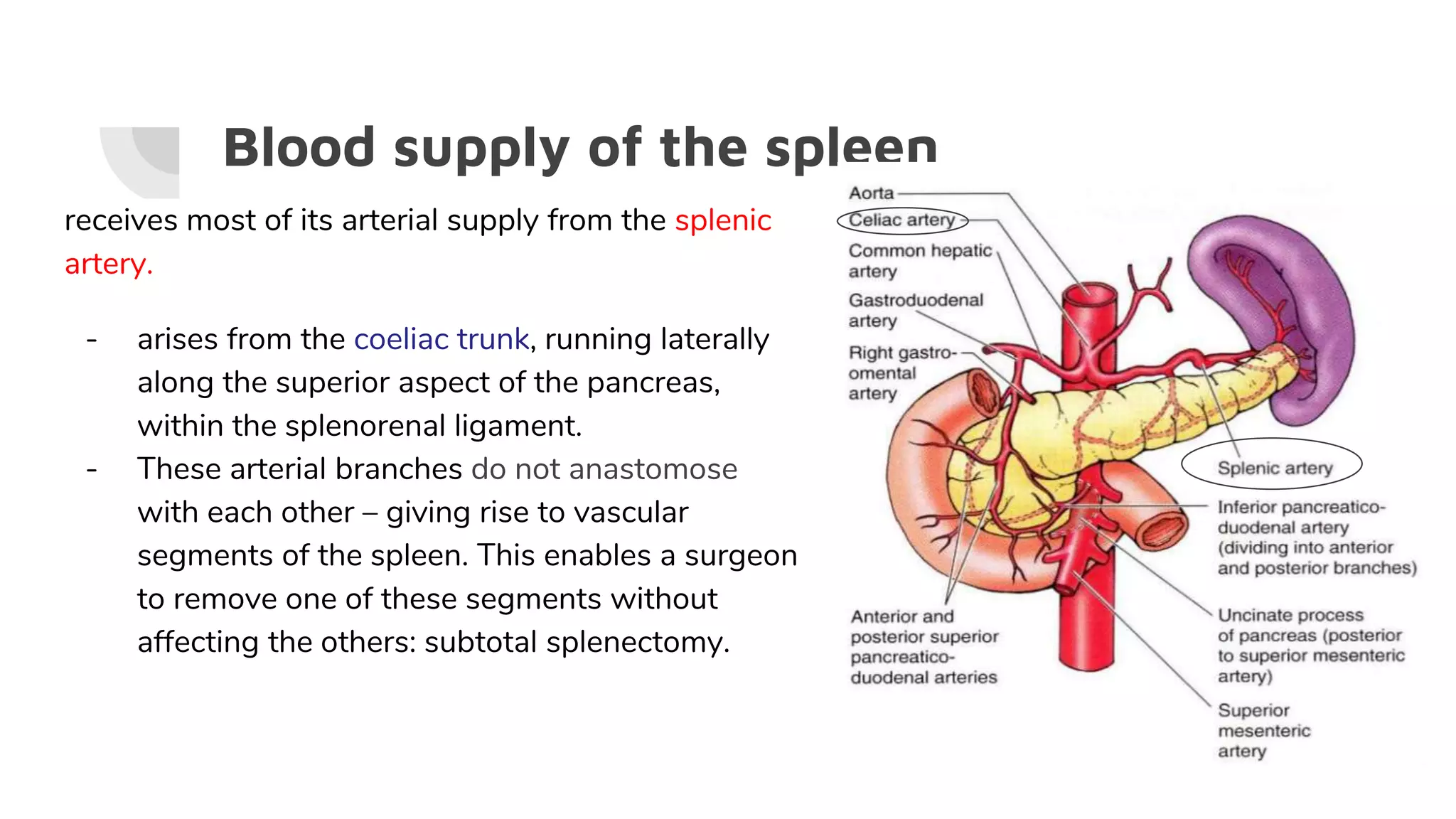
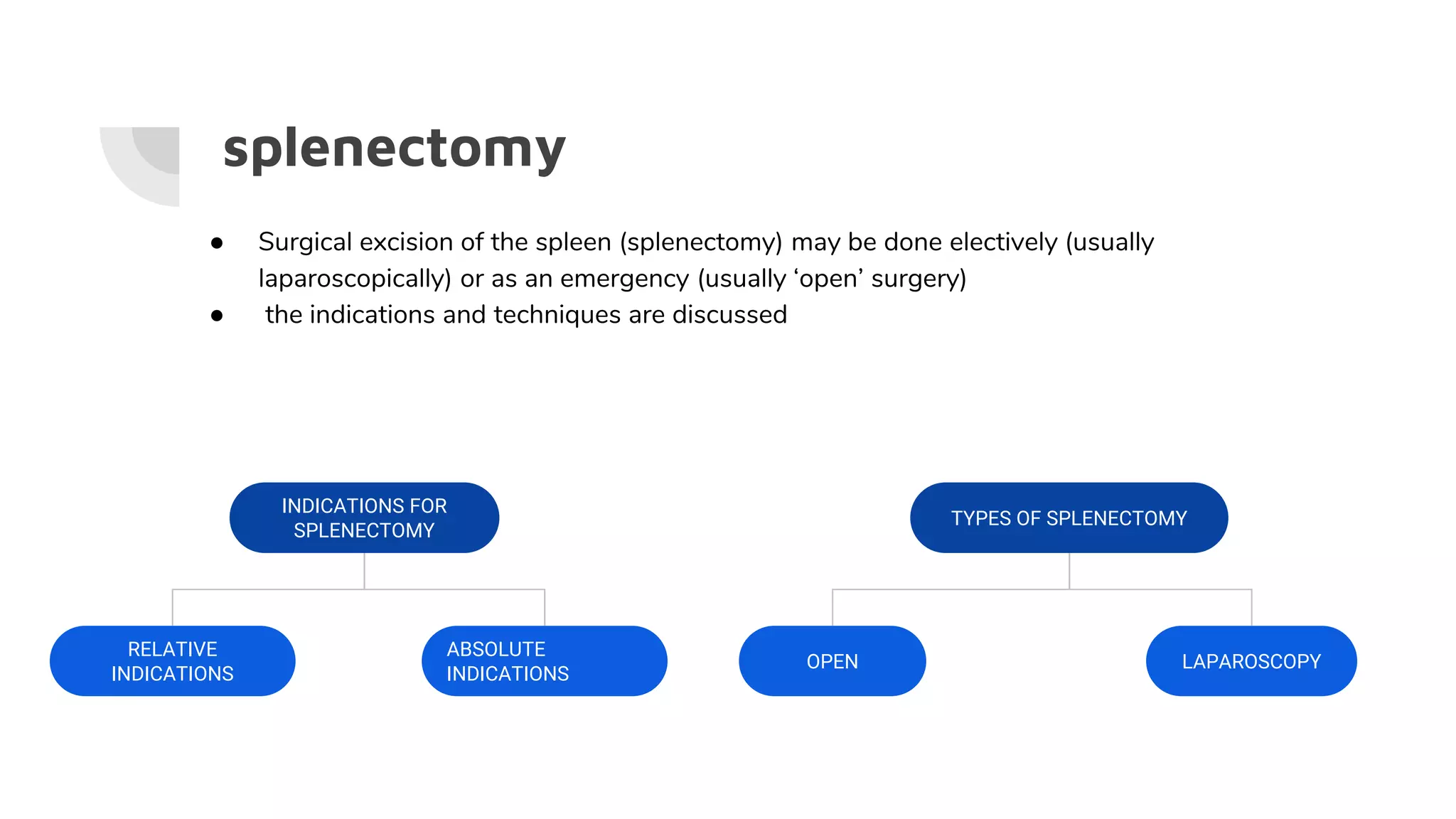
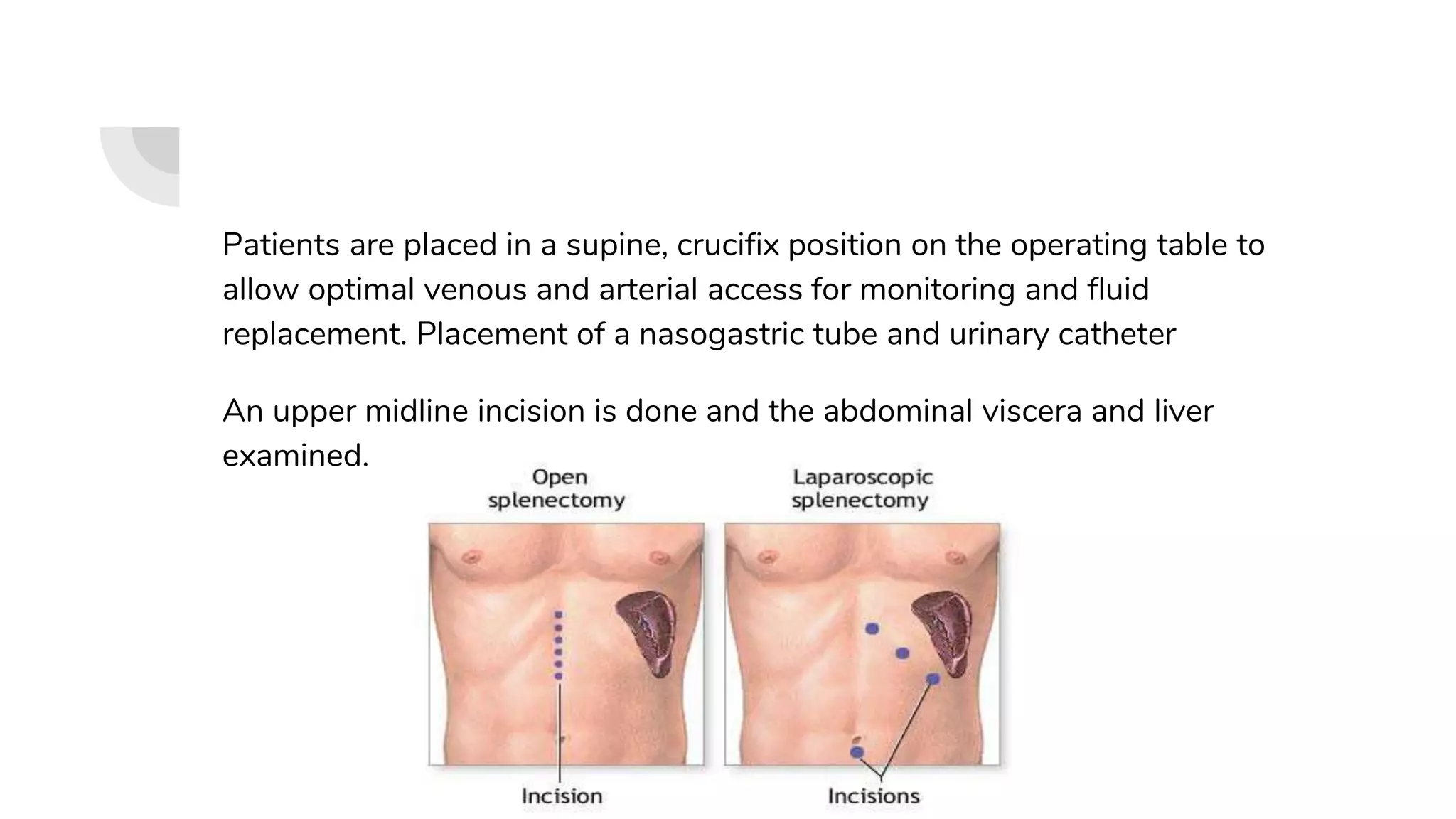
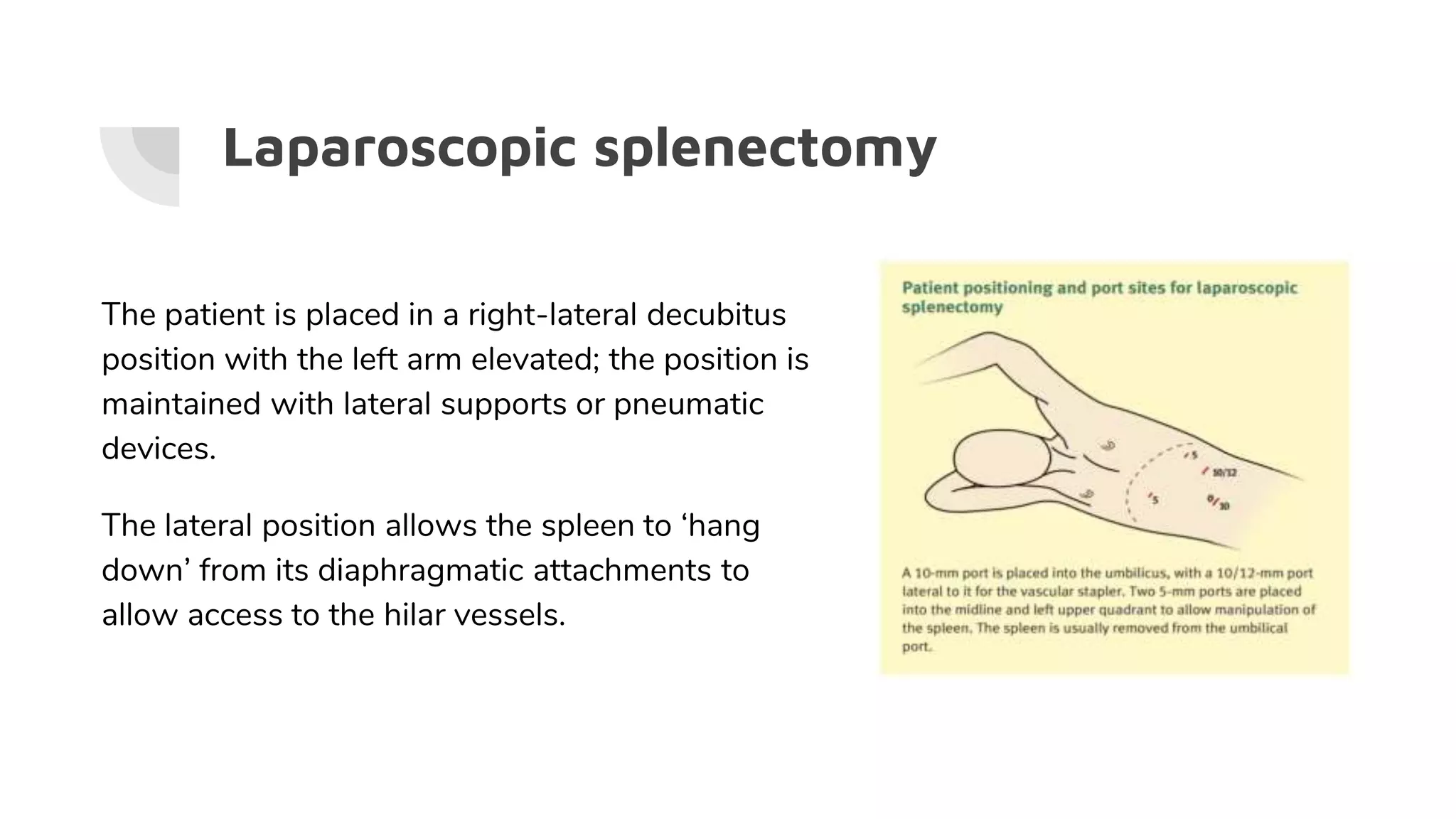
The spleen is responsible for filtering blood and mounting immune responses. Indications for splenectomy include trauma, idiopathic thrombocytopenic purpura refractory to steroids, and hematological conditions causing abnormal red blood cell morphology. Splenectomy may be performed open or laparoscopically and indications include trauma, hematological diseases, neoplasms, and spontaneous rupture. Complications include infection, bleeding, and thrombocytosis.