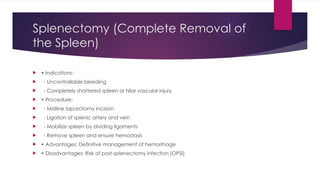
Blunt abdominal trauma can lead to splenic rupture, which is the most common injury to solid organs in such cases and can cause life-threatening bleeding. Non-operative management is recommended for hemodynamically stable patients, while surgical intervention, such as splenectomy, is necessary for unstable cases or major injuries. Post-splenectomy care includes vaccinations and monitoring for overwhelming post-splenectomy infection (OPSI), which has high mortality if not managed promptly.

![SPLENIC RUPTURE
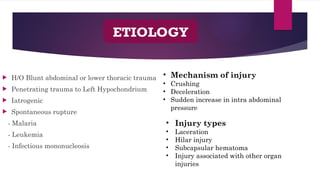
Splenic rupture can occur as trauma to normal spleen or
diseased spleen
Atraumatic rupture of a diseased spleen [pathologic rupture]
and spontaneous rupture of normal spleen [spontaneous
idiopathic rupture]
Spleen is the most common solid organ injured in blunt injury
abdomen
Classically associated with left lower ribs fracture
Delayed rupture is a characteristic feature in Subcapsular
hematoma
A ruptured spleen can cause life-threatening bleeding into the
abdominal cavity.](https://image.slidesharecdn.com/splenictrauma110907-250131033452-f60f2dfa/85/splenic-trauma-grading-and-it-s-management-2-320.jpg)