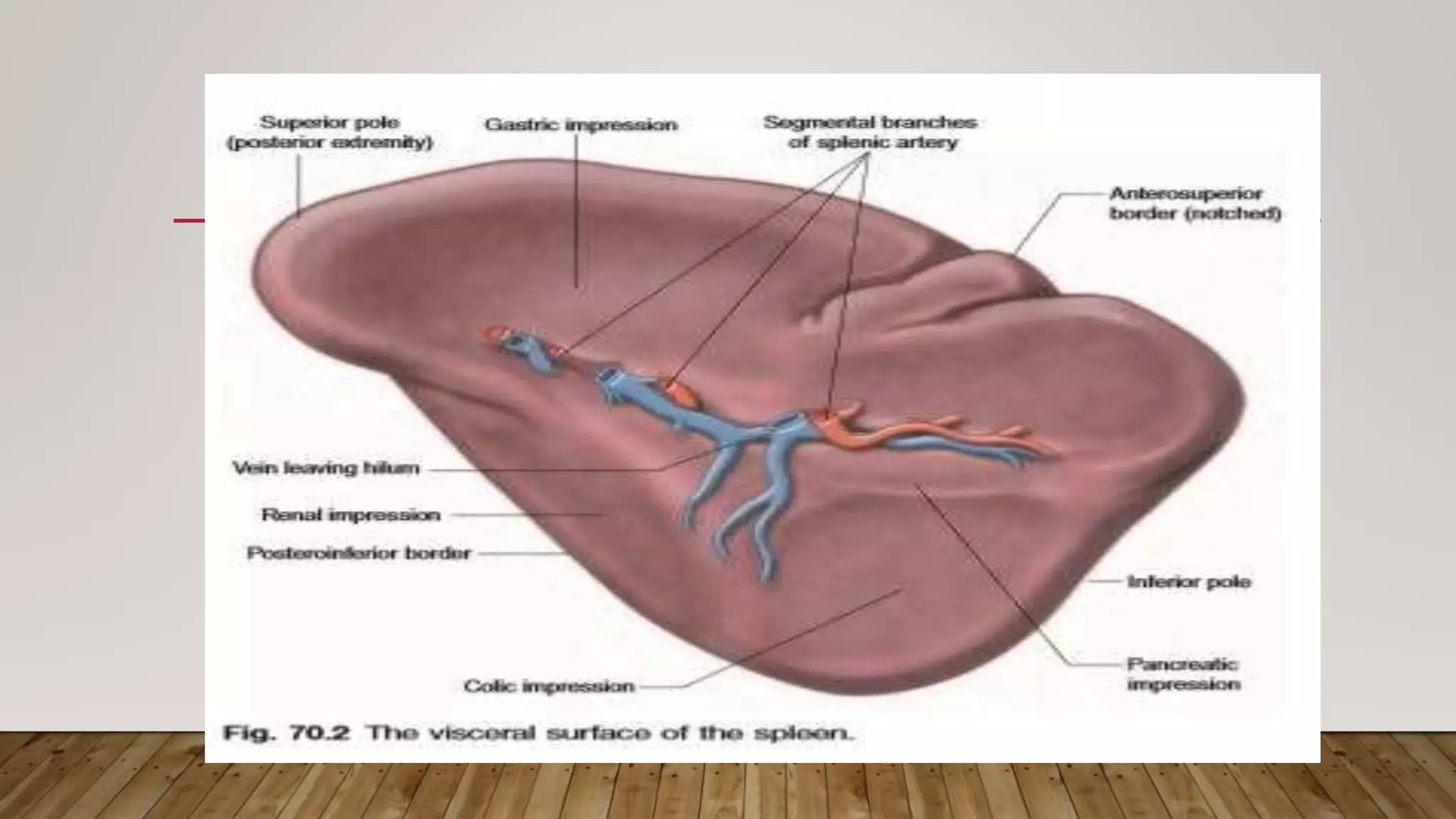
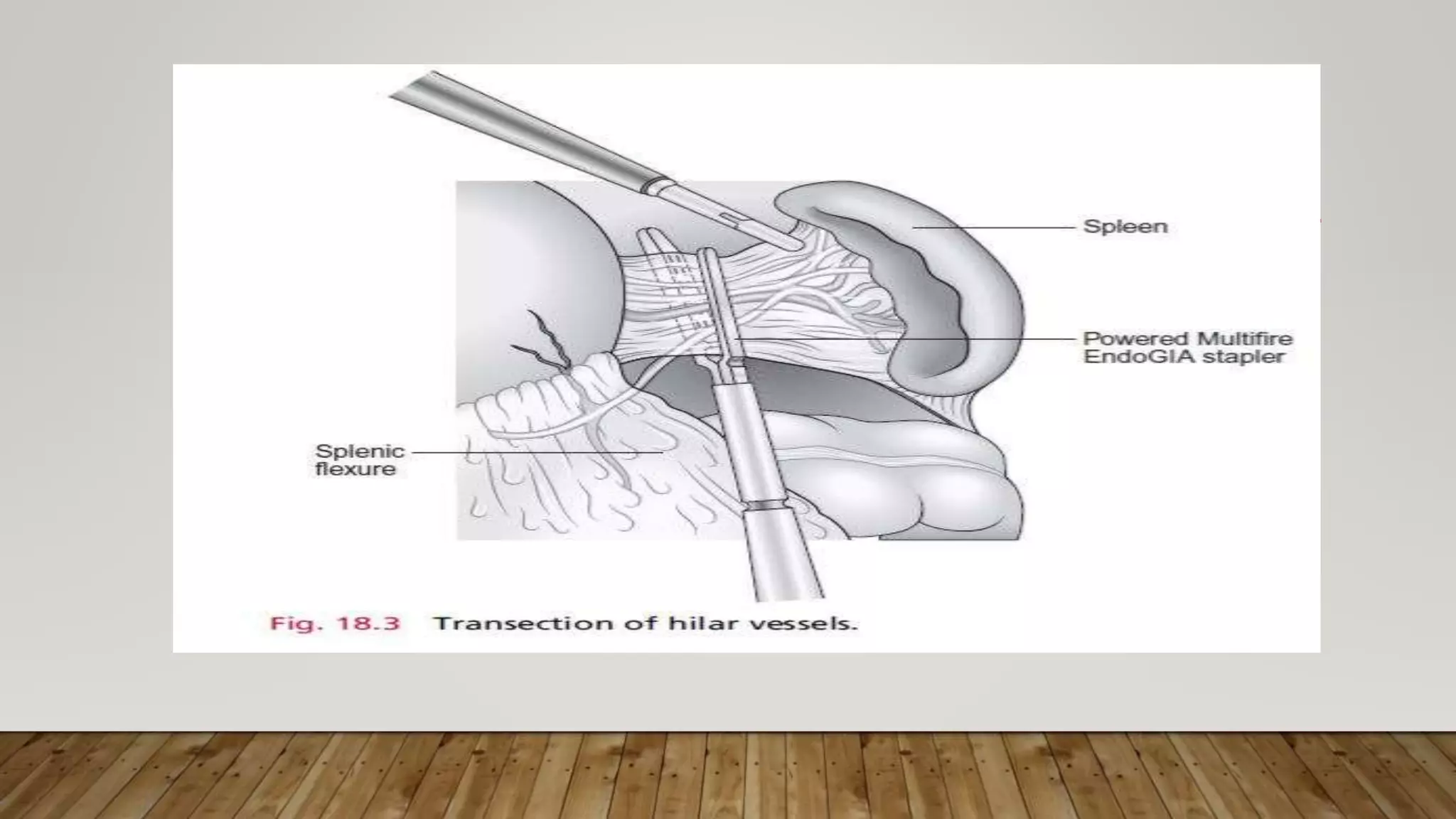
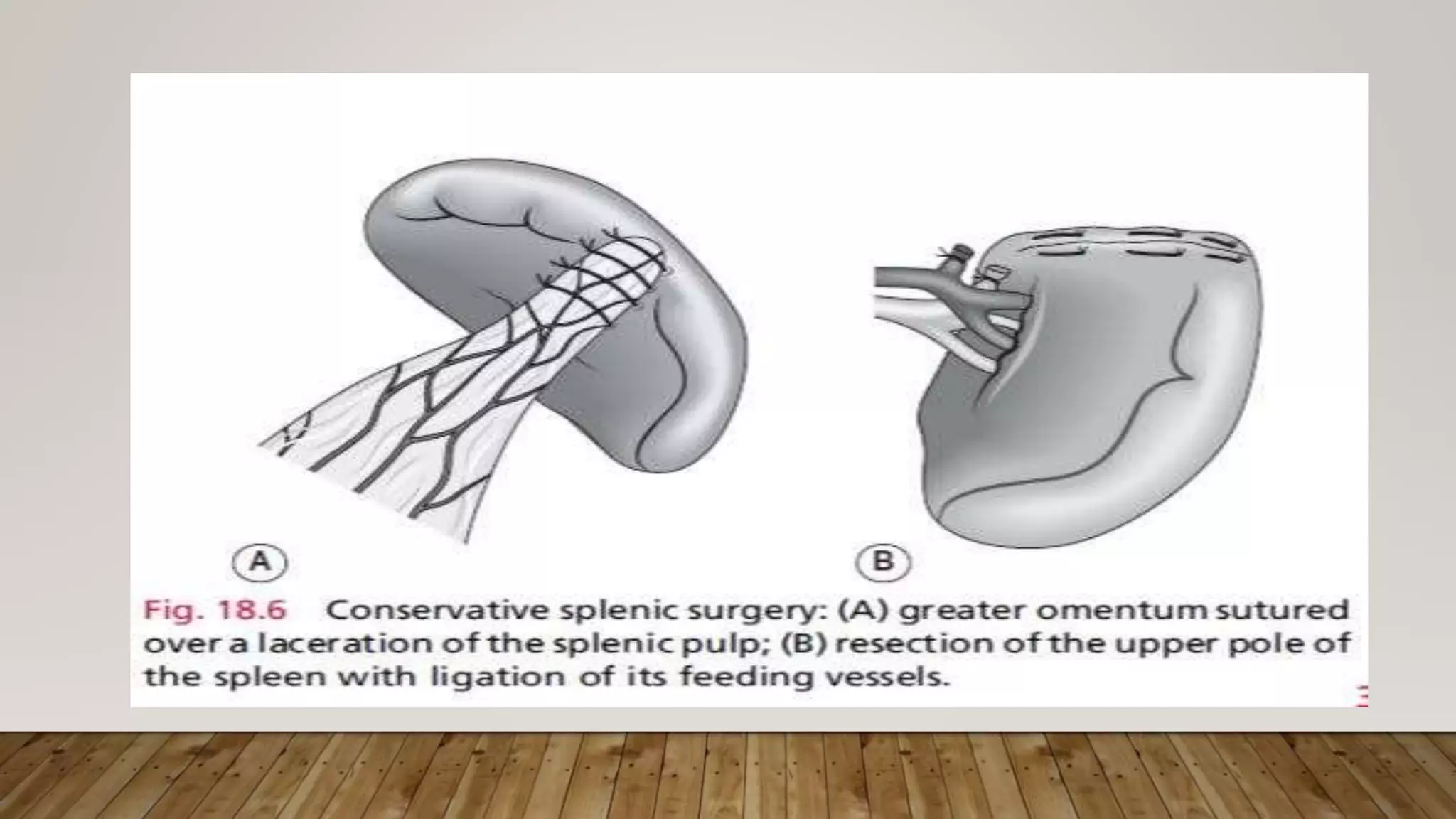
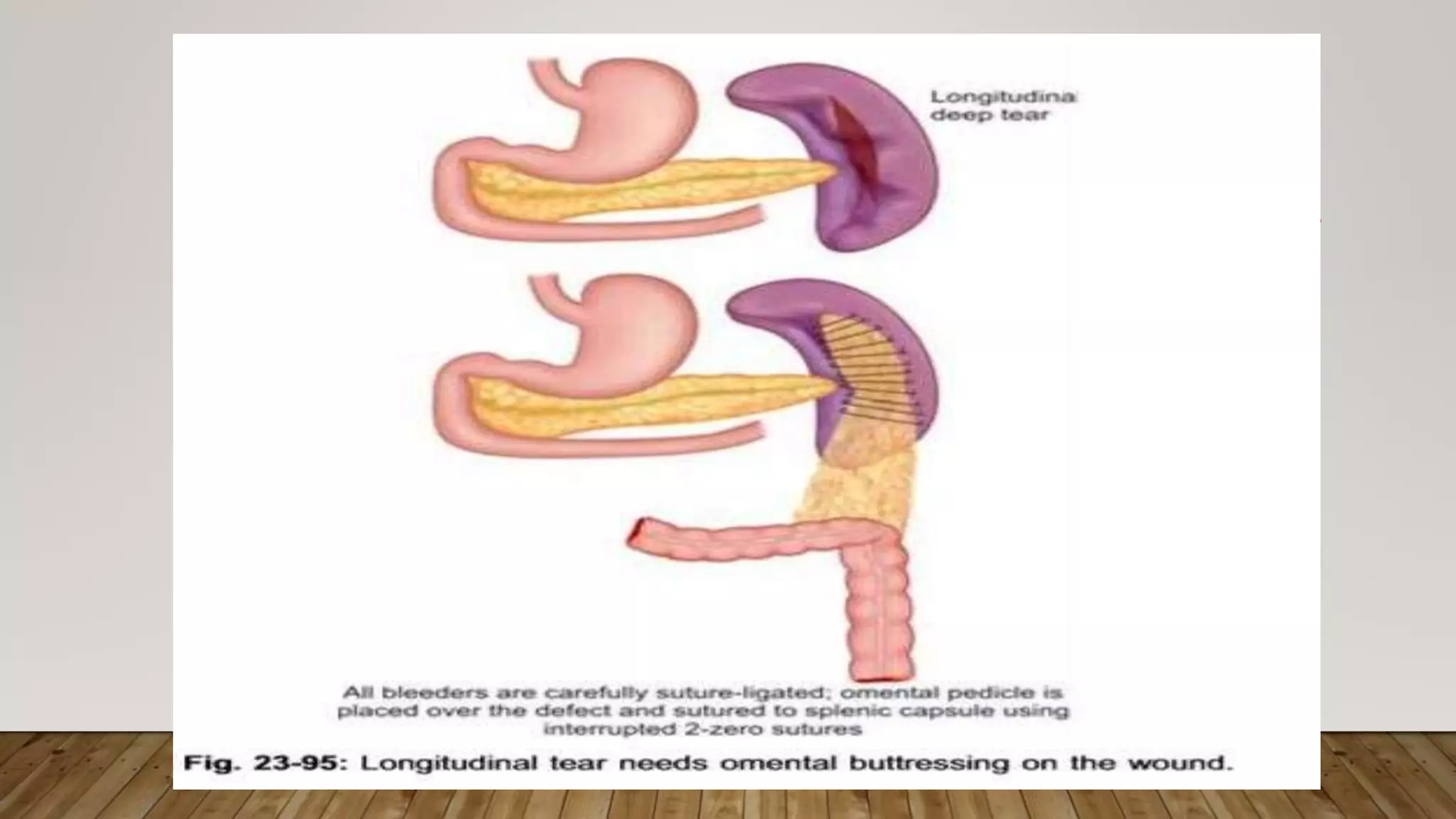
The spleen is an organ located in the upper left abdomen. It filters blood and fights infections. A splenectomy is the surgical removal of the spleen. It is usually performed laparoscopically to avoid complications of open surgery. During the procedure, the surgeon uses cameras and surgical tools inserted through small incisions to carefully dissect and divide attachments of the spleen. This allows the spleen to be removed while preserving surrounding structures like the pancreas and stomach. A splenectomy may be recommended for conditions like immune thrombocytopenia or certain blood disorders.