The document discusses the history of wound care from ancient times to modern practices. Some key points covered include:
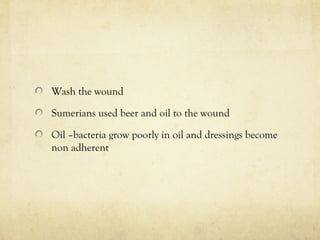
- Ancient civilizations used remedies like honey, grease, and herbs to treat wounds. Hippocrates advocated cleaning wounds with wine or vinegar.
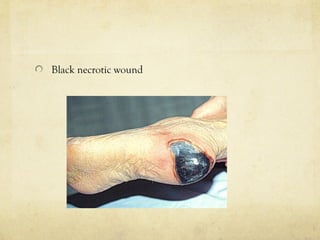
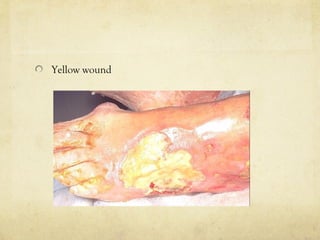
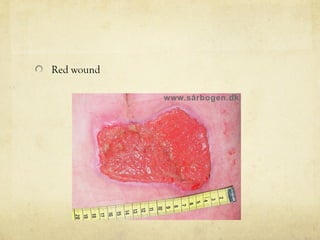
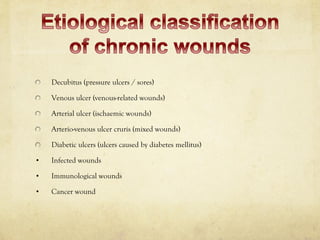
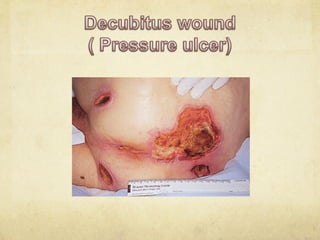
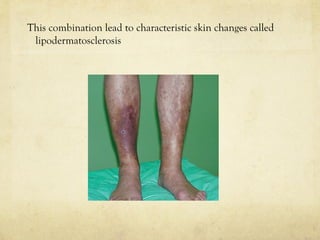
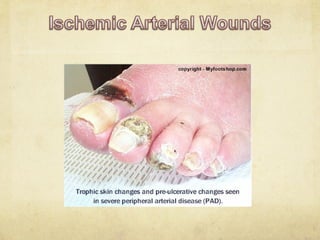
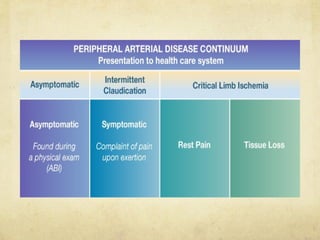
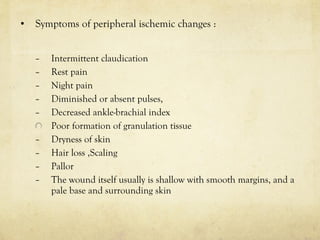
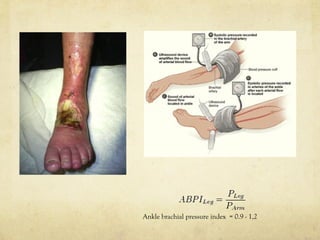
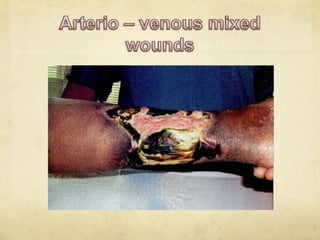
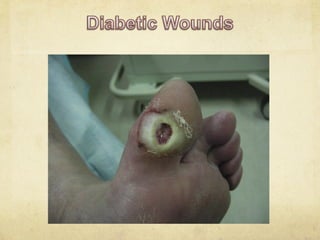
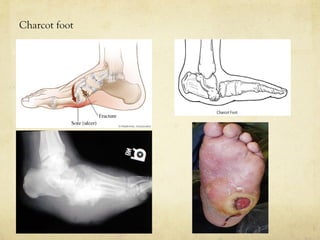
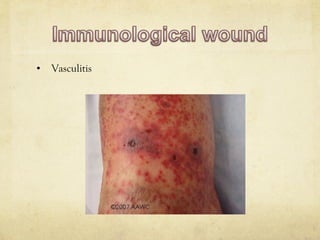
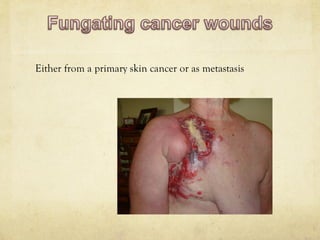
- Different types of wounds are discussed like acute, chronic, pressure ulcers, venous ulcers, and diabetic foot ulcers.
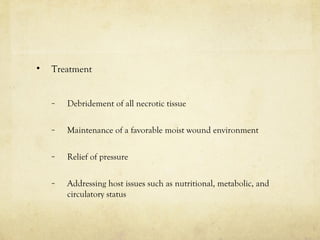
- Modern wound care includes debridement, dressings, antibiotics, growth factors, skin substitutes, and addressing underlying patient issues.
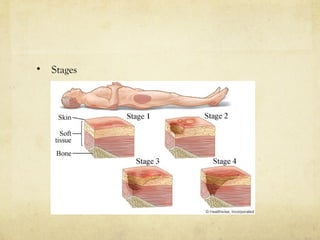
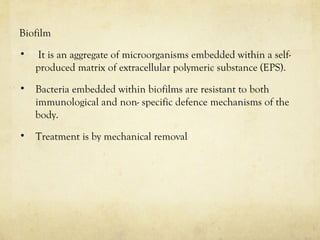
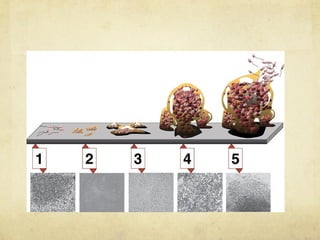
- Wound etiology, staging, and treatments are described for various chronic wounds. Biofilms, infection, and other complex wound factors are also addressed.