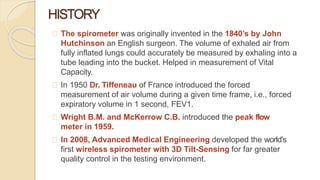
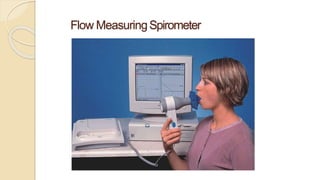
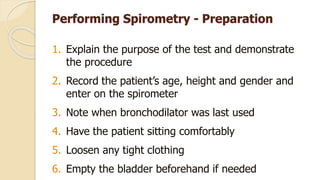
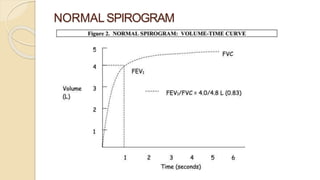
Spirometry is a lung function assessment method that measures the volume of air a patient can expel after maximal inspiration, with historical development dating back to the 1840s. It is primarily used for diagnosing conditions like asthma and COPD, evaluating airflow obstruction, and monitoring disease progression. The test involves specific preparation, execution, and may have side effects, with various types of spirometers available for different settings.