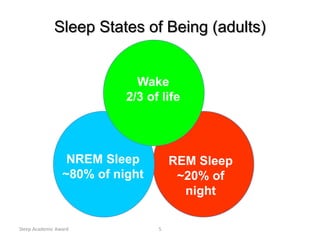
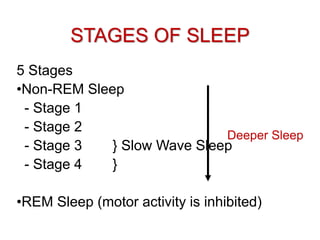
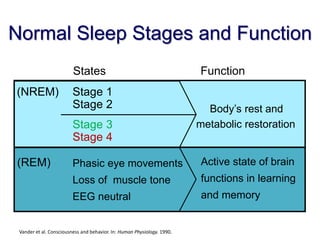
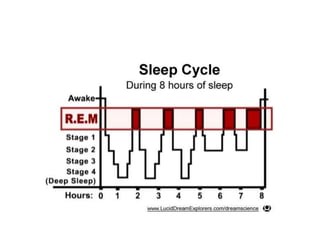
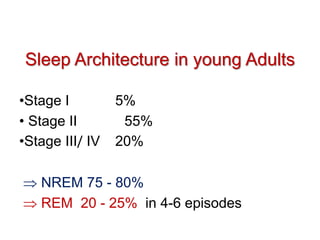
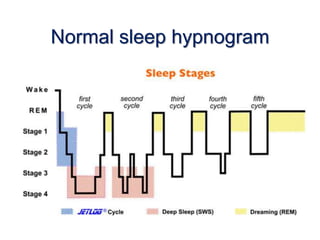
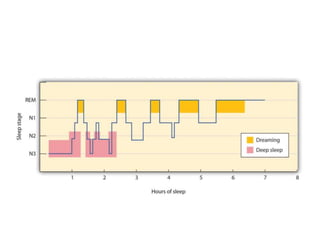
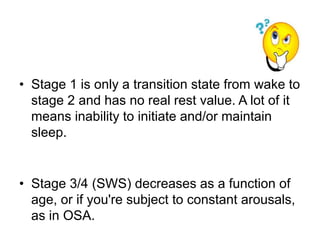
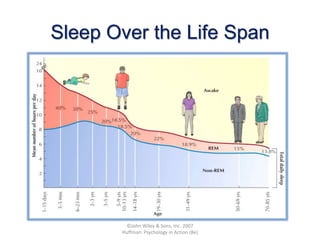
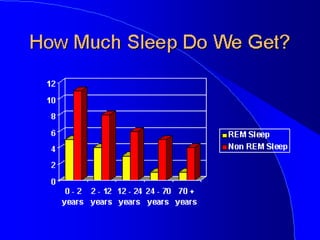
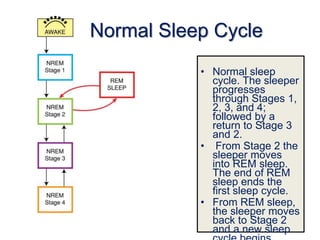
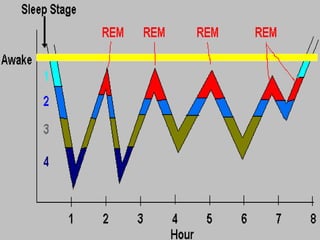
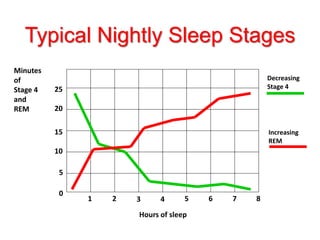
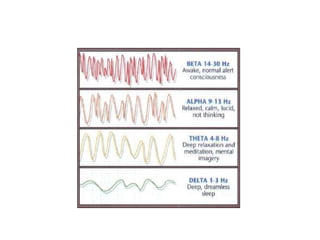
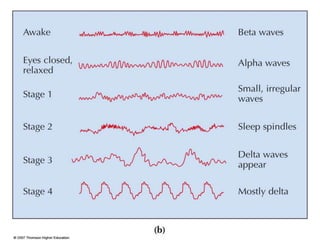
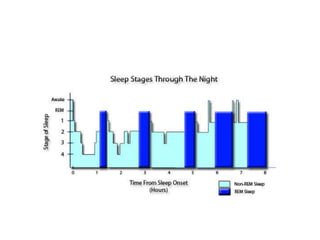
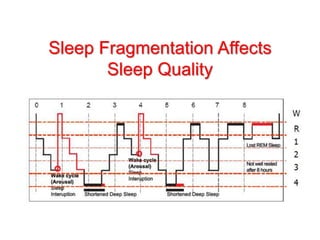
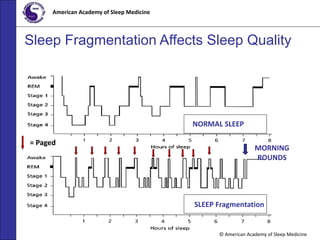
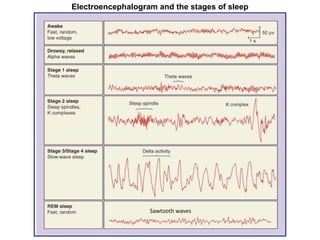
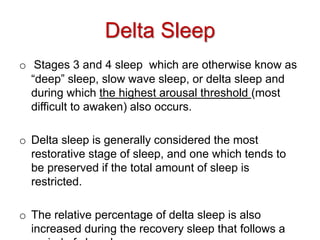
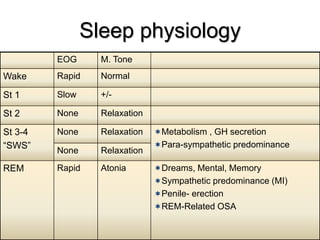
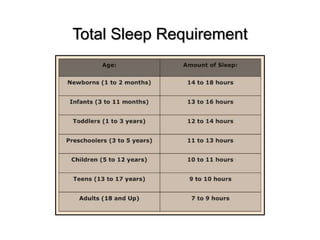
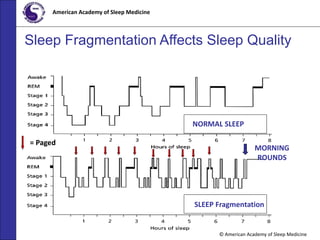
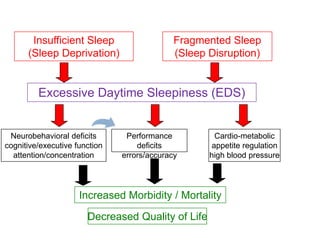
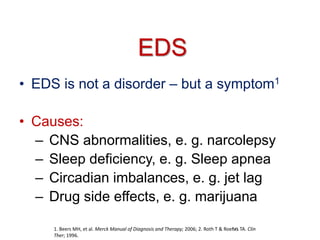
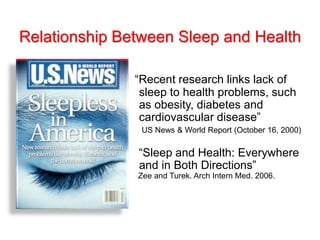
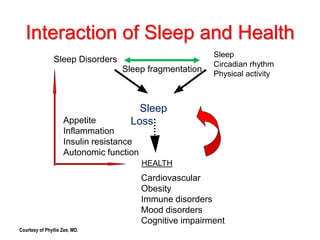
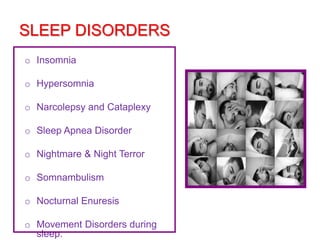
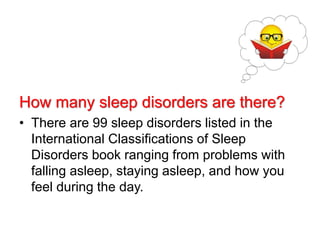
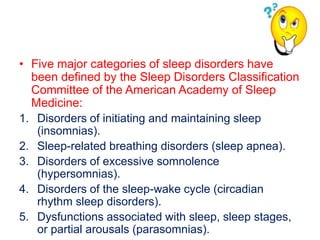
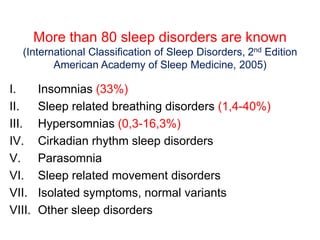
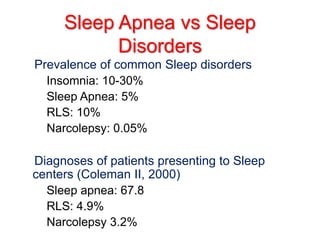
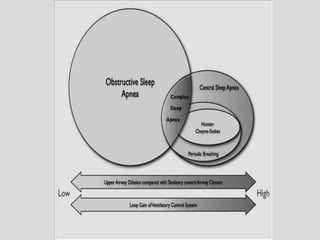
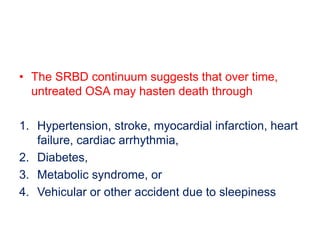
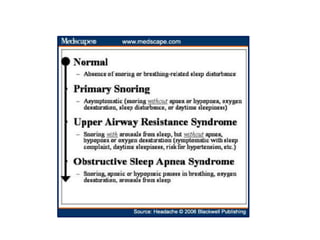
Sleep progresses through stages including REM sleep and NREM sleep. NREM sleep includes stages 1-4, with stages 3 and 4 being slow wave or deep sleep. A normal sleep cycle lasts 90-110 minutes and progresses from light to deep sleep and then to REM sleep before repeating. Lack of sleep or fragmented sleep can negatively impact health by reducing time in restorative sleep stages and increasing daytime sleepiness. Common sleep disorders include insomnia, sleep apnea, hypersomnias, and circadian rhythm disorders.