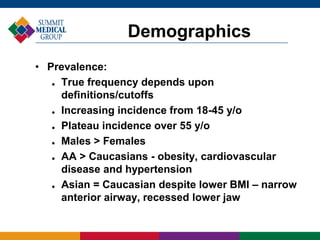
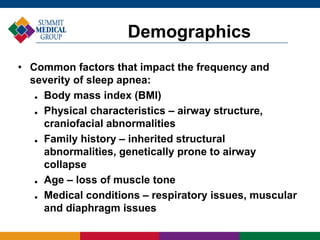
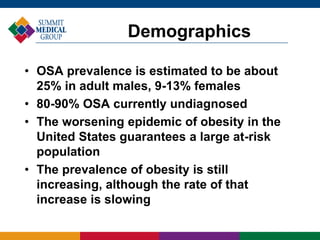
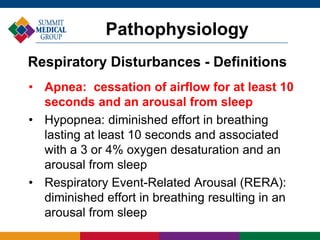
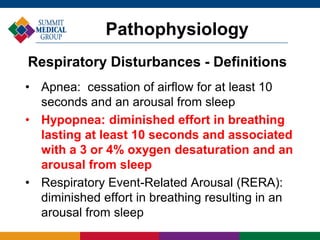
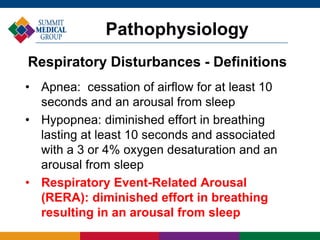
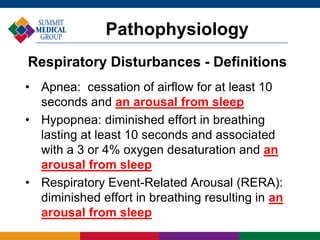
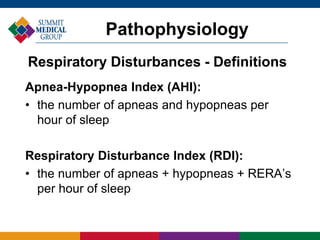
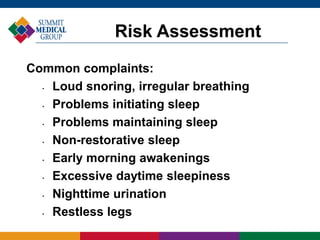
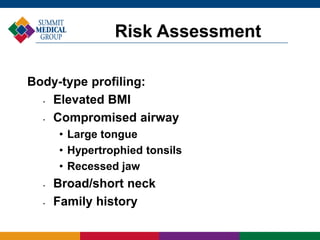
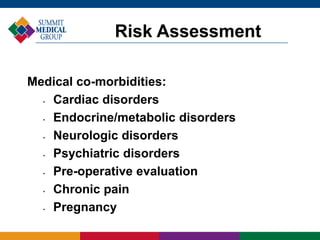
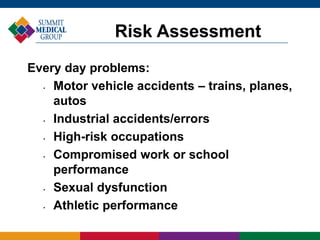
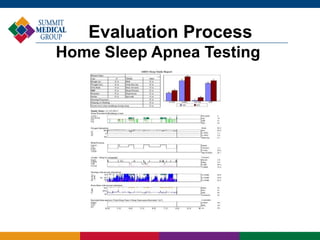
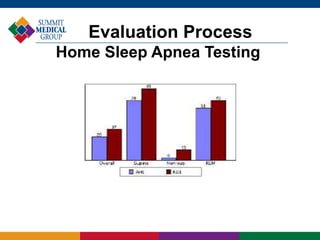
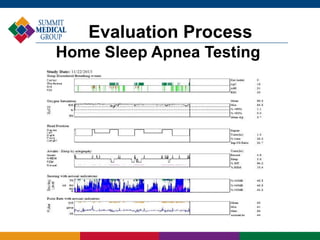
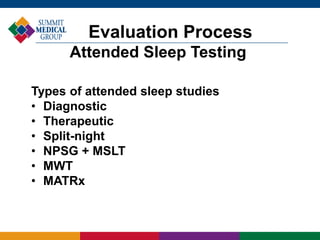
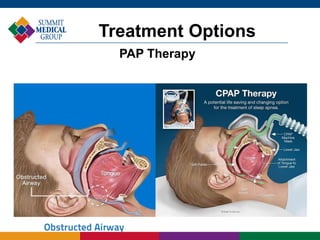
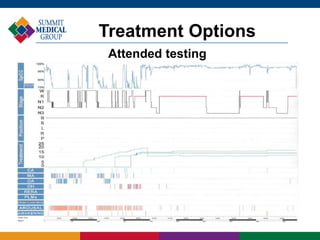
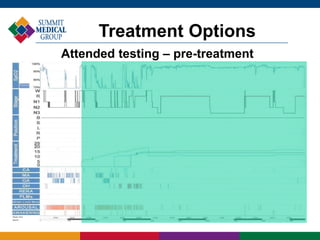
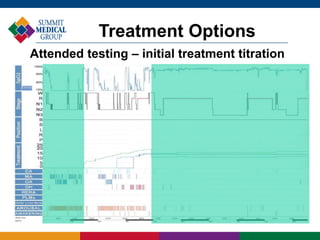
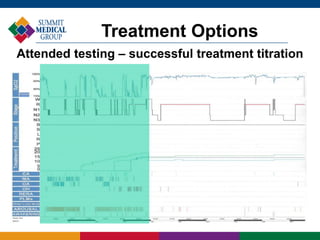
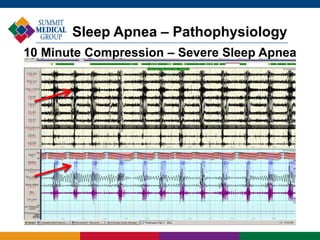
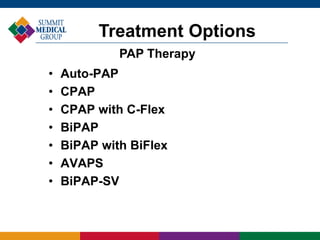
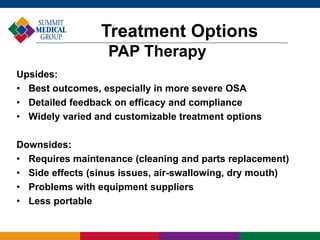
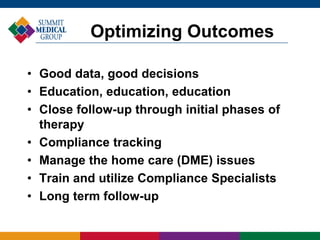
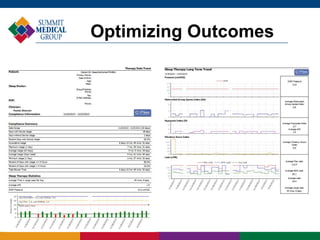
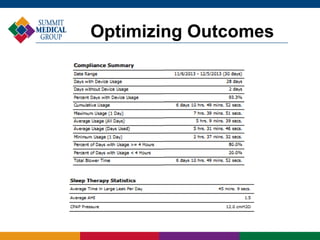
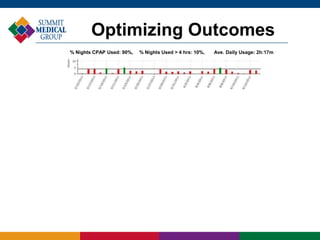
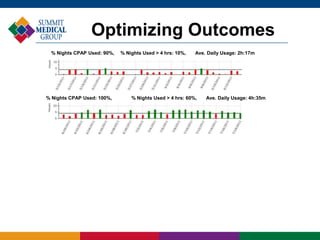
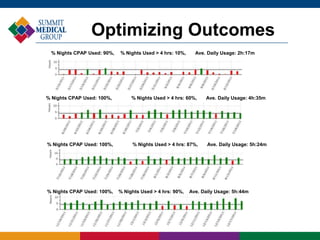
The document provides an overview and update on sleep apnea, including its evaluation and treatment. It discusses the definition and types of sleep apnea, risk factors, diagnostic testing options, and treatment approaches such as CPAP, oral appliances, surgery, and lifestyle changes. The key goals in managing sleep apnea are to obtain accurate diagnostic data, educate patients, closely monitor treatment adherence, address any equipment issues, and ensure long-term follow up to optimize outcomes.