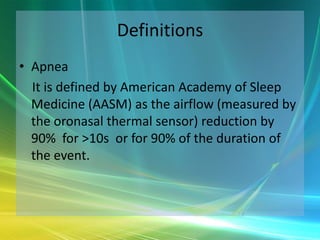
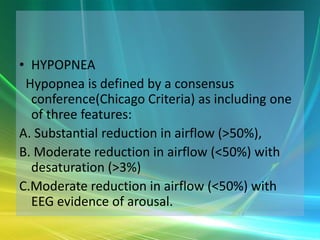
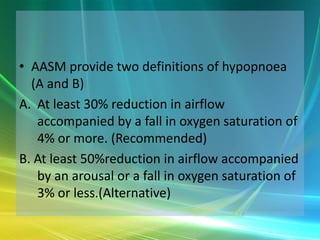
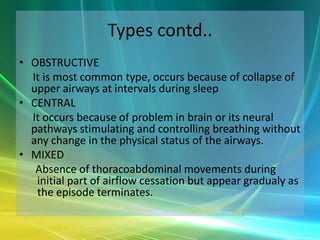
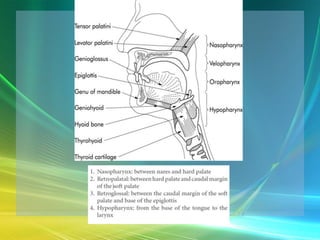
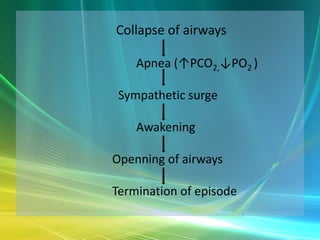
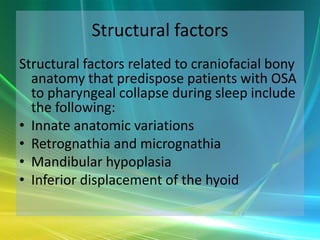
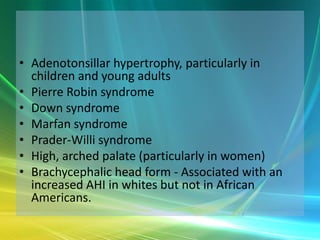
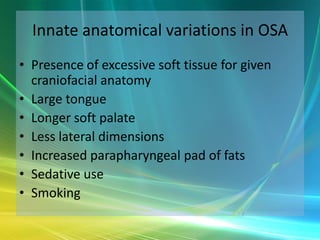
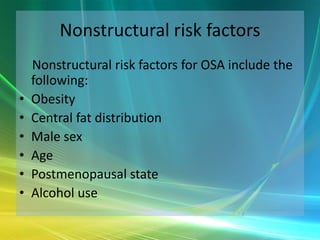
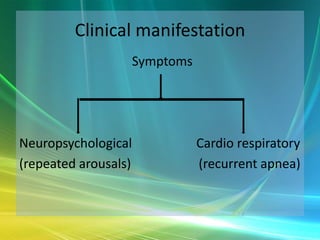
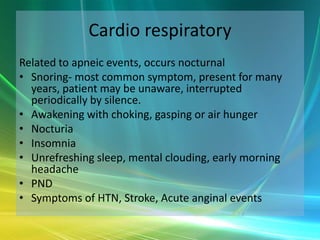
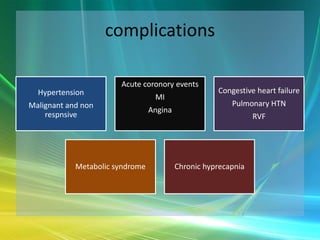
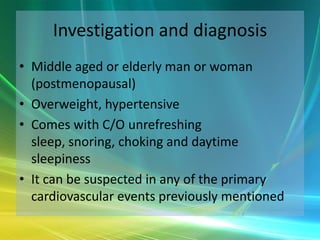
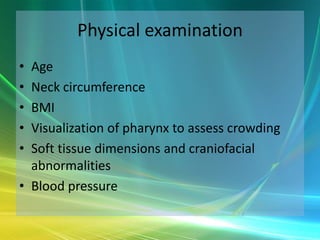
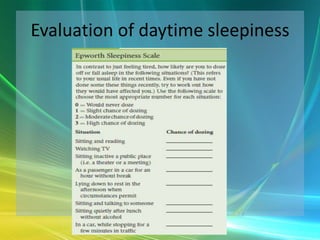
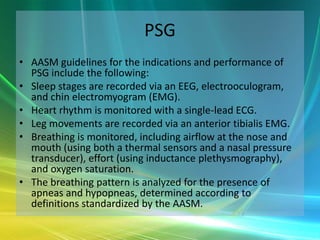
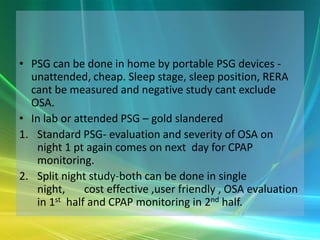
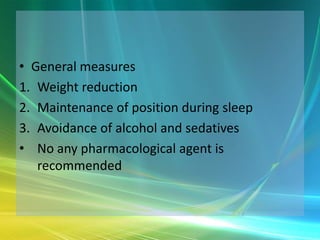
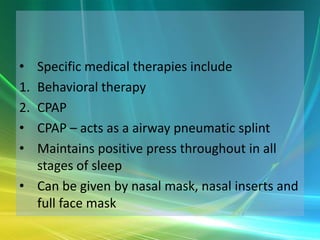
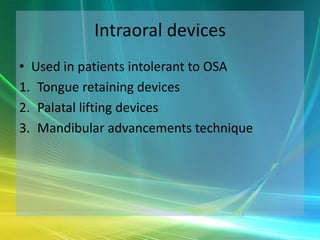
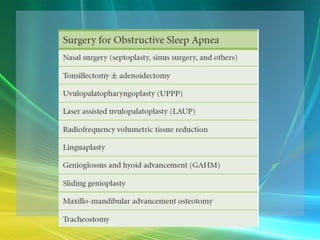
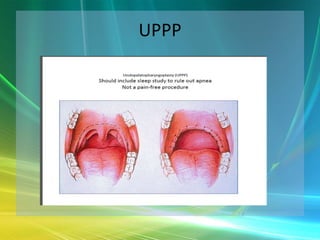
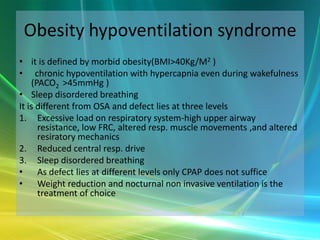
This document defines and describes sleep apnea, its types (obstructive, central, mixed), risk factors, symptoms, complications, diagnosis via polysomnography (PSG), and treatment options including weight loss, CPAP, oral devices, surgery, and management of obesity hypoventilation syndrome. Sleep apnea is characterized by pauses in breathing during sleep caused by airway collapse and is associated with daytime sleepiness and cardiovascular issues. PSG is the gold standard test to evaluate sleep architecture and breathing disturbances. Treatment focuses on maintaining an open airway through lifestyle changes and devices.