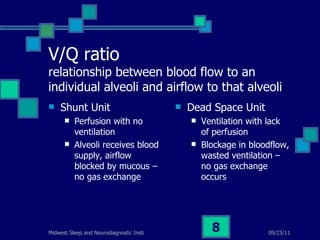
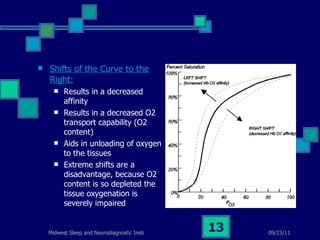
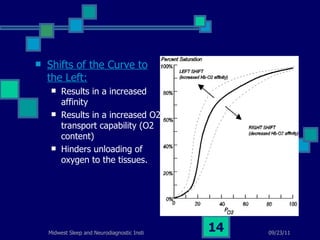
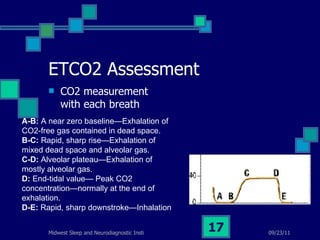
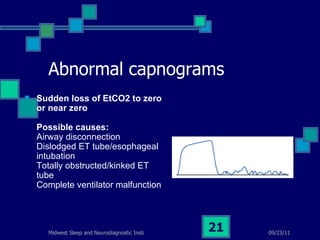
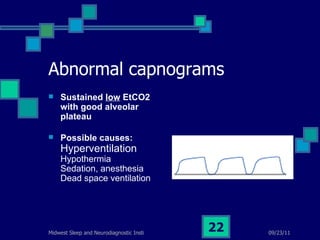
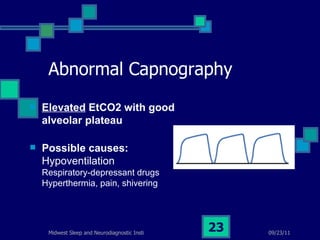
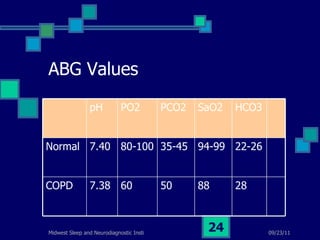
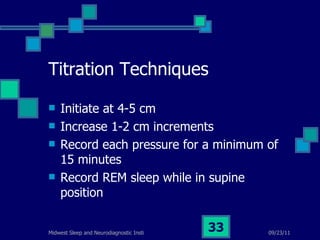
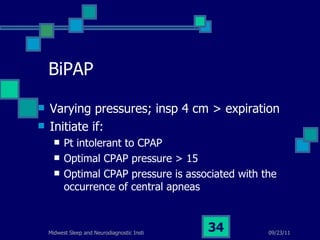
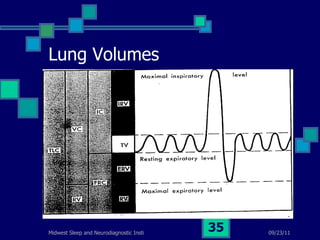
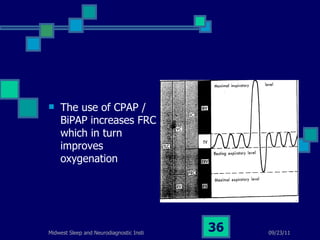
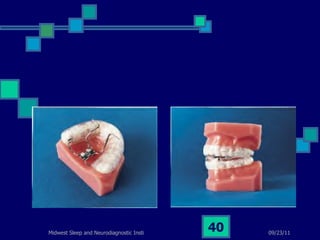
Sleep disordered breathing refers to conditions like obstructive sleep apnea that disrupt normal breathing patterns during sleep. Key factors that influence gas exchange in the lungs include the V/Q ratio and the oxygen dissociation curve. Treatment options for obstructive sleep apnea include CPAP/BiPAP devices, oral appliances, and surgeries like uvulopalatopharyngoplasty. Capnography and end-tidal carbon dioxide measurements provide important windows into a patient's ventilation.