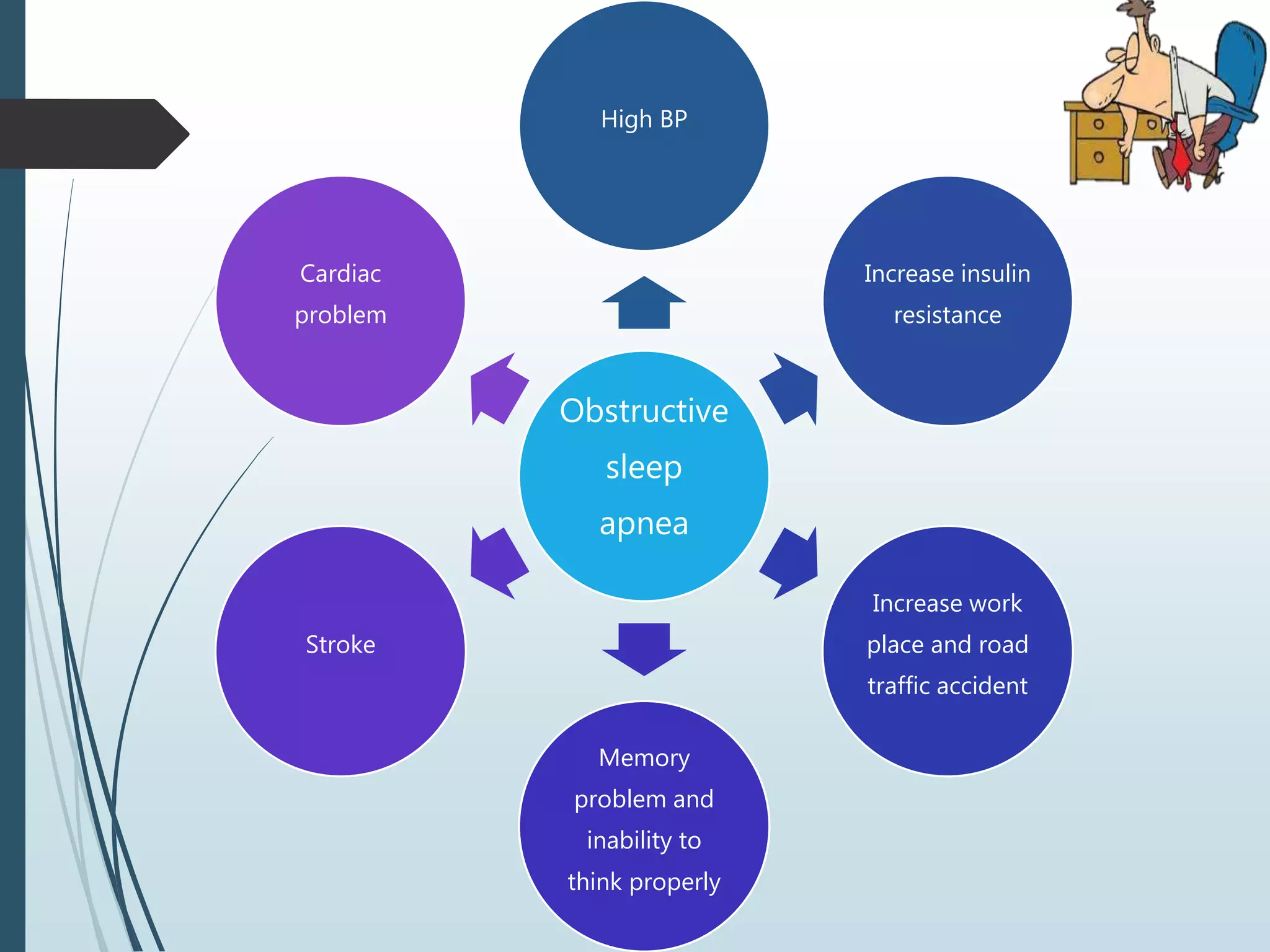
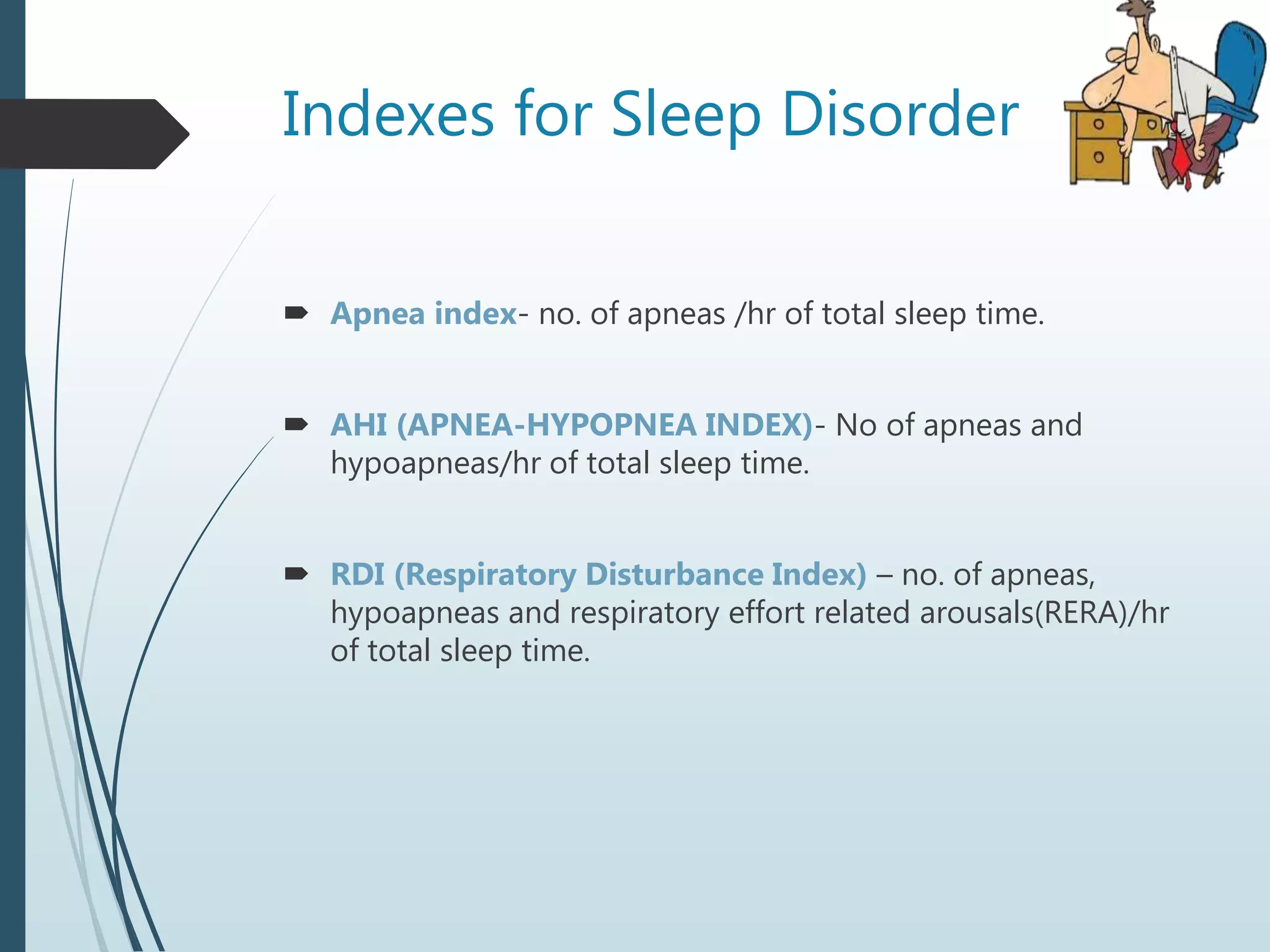
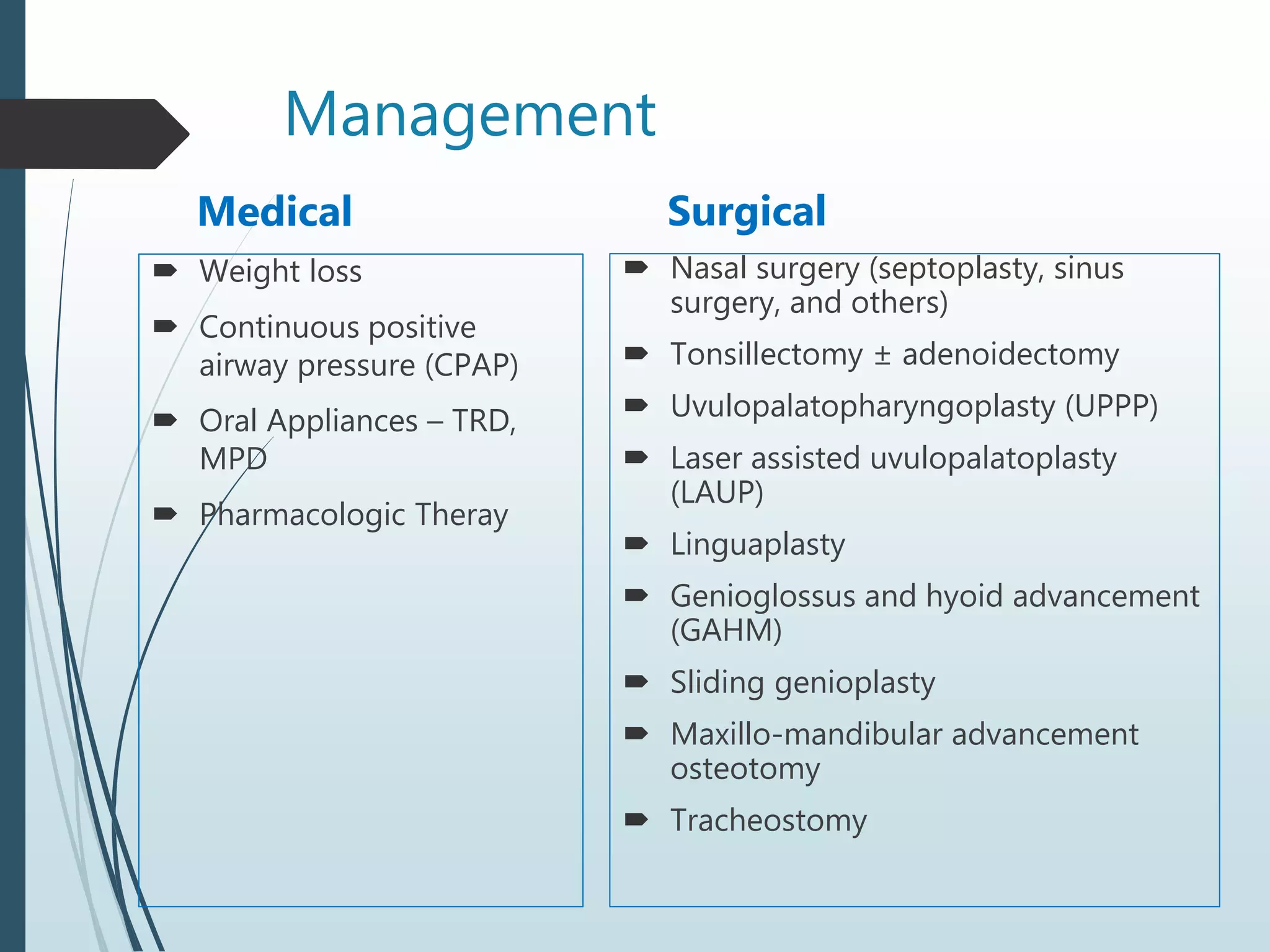
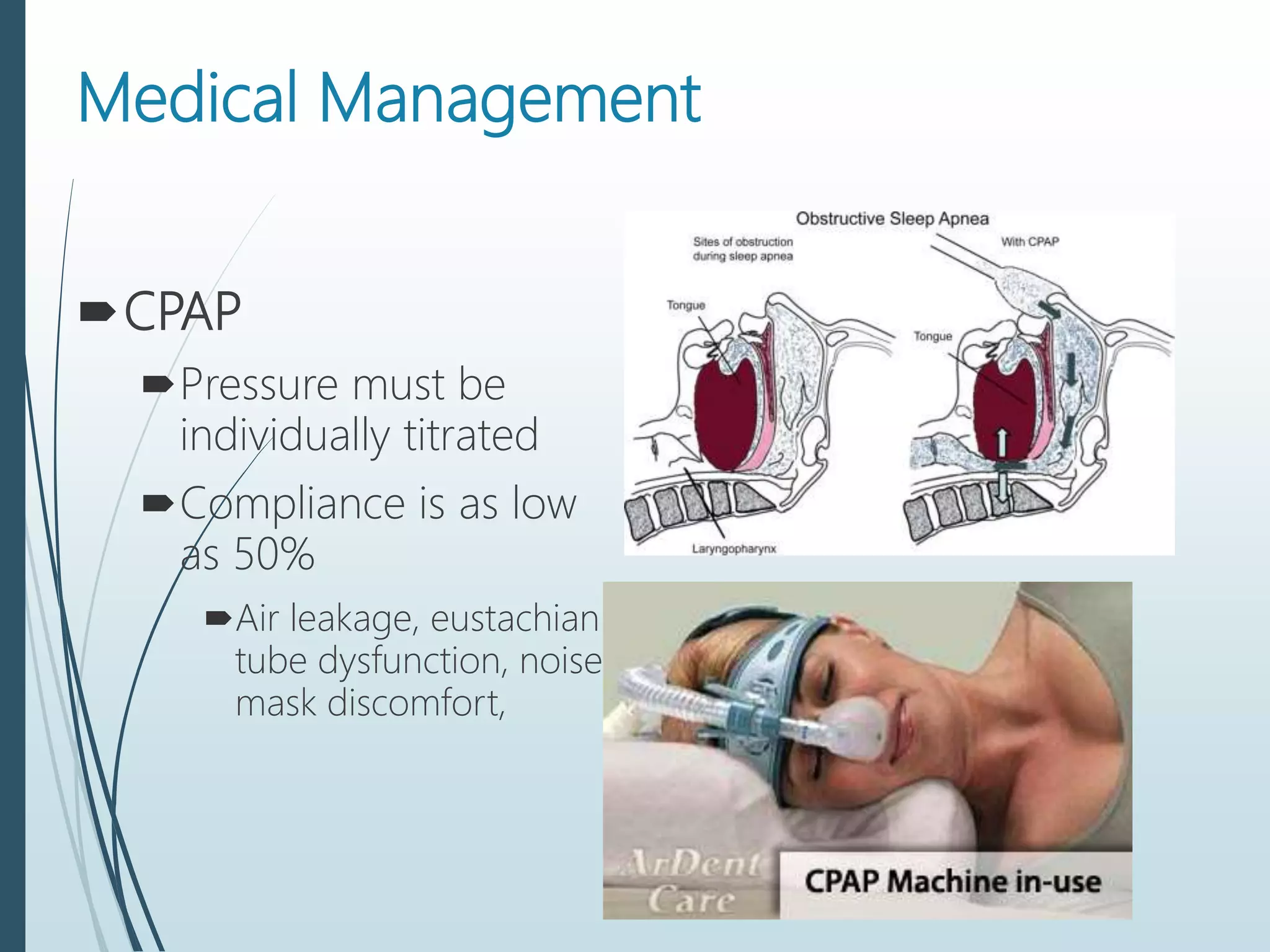
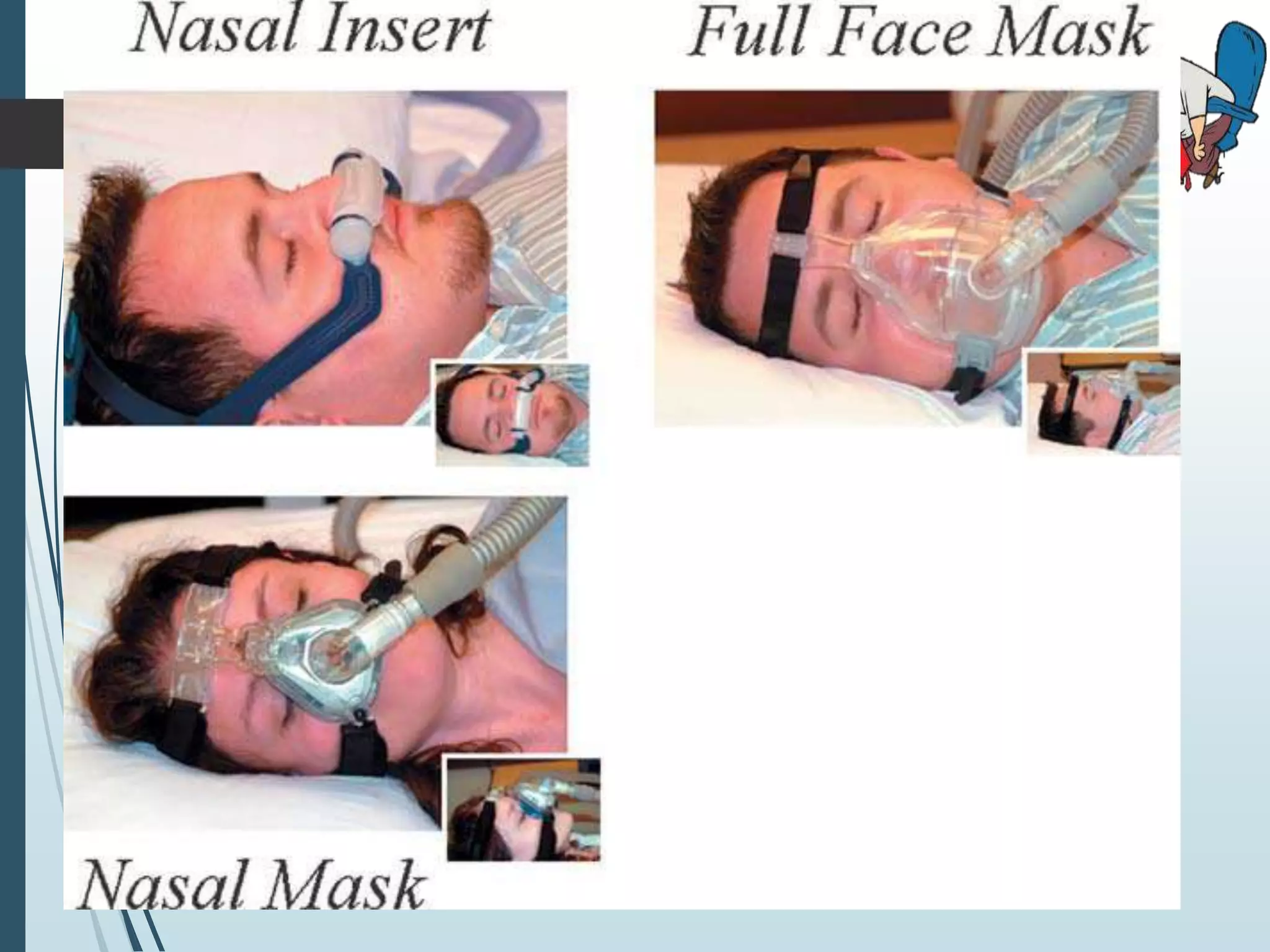
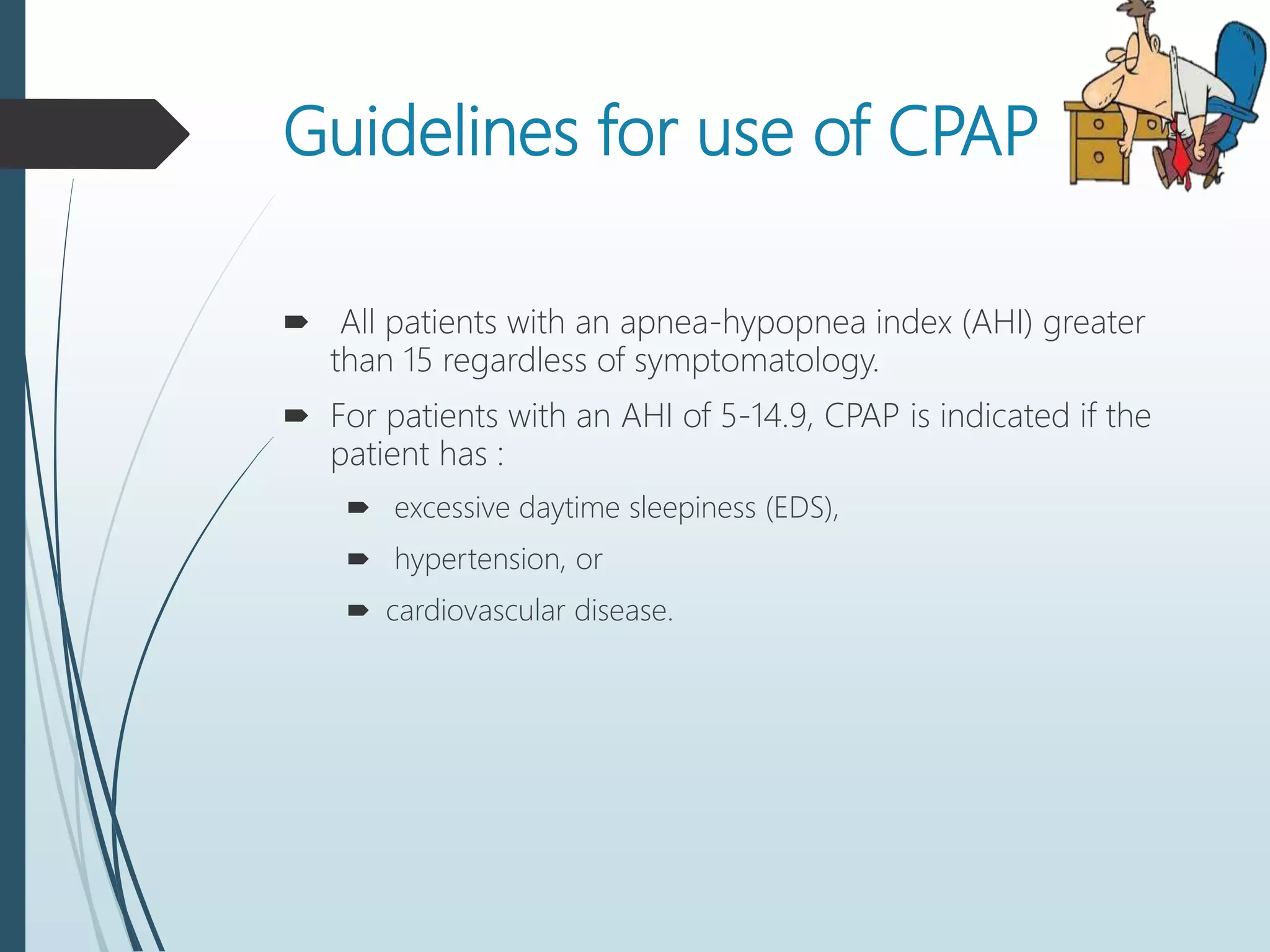
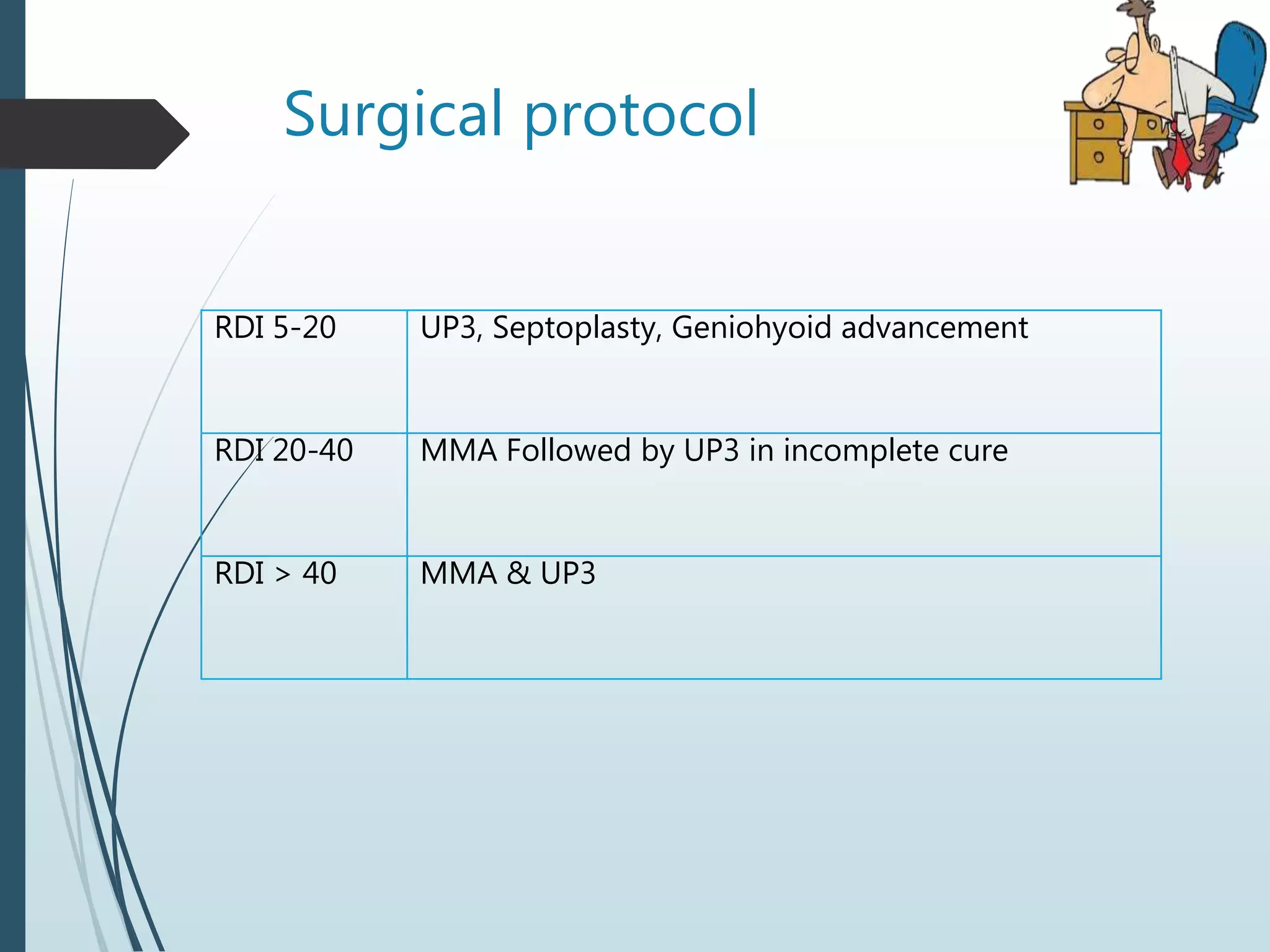
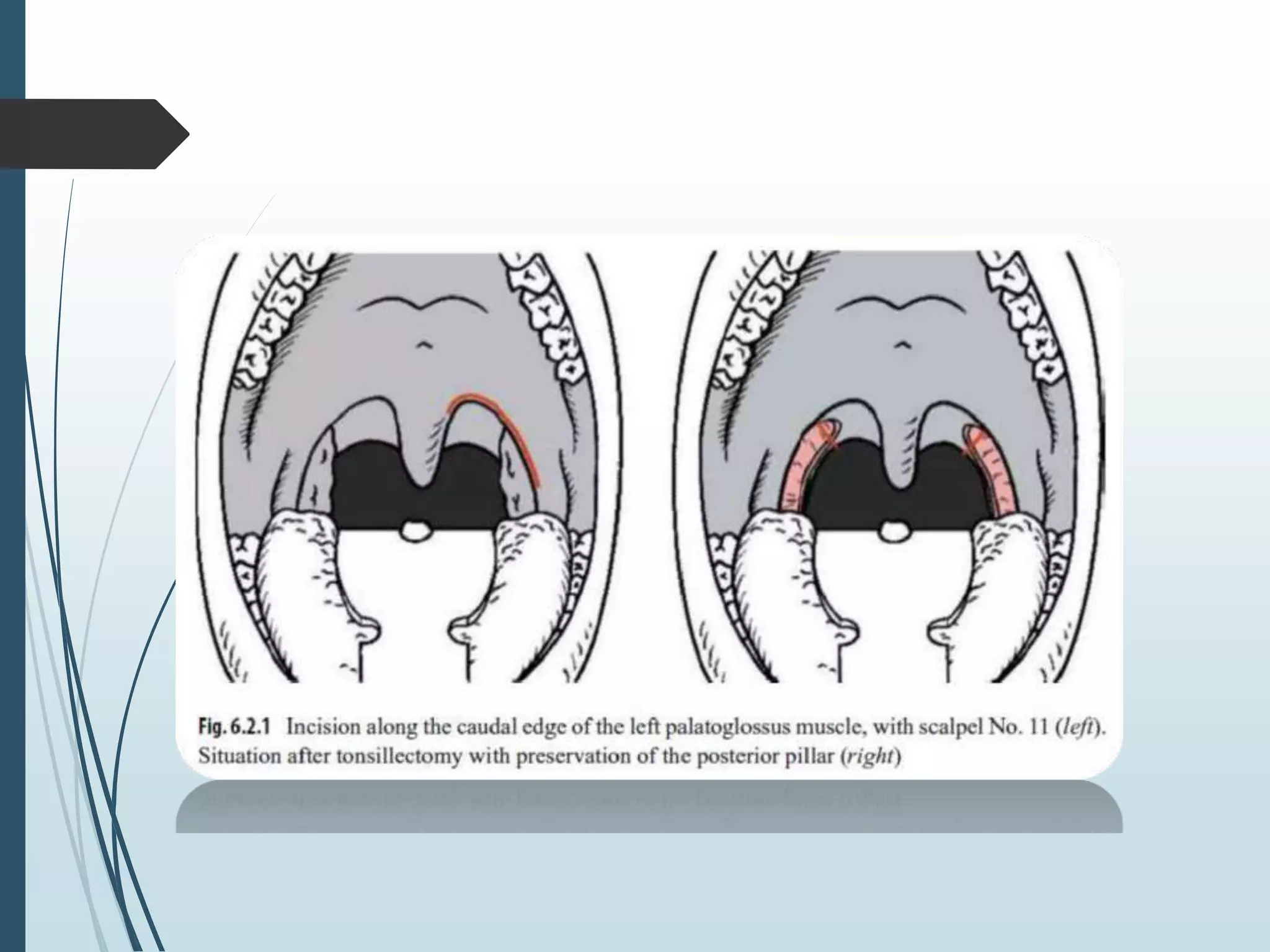
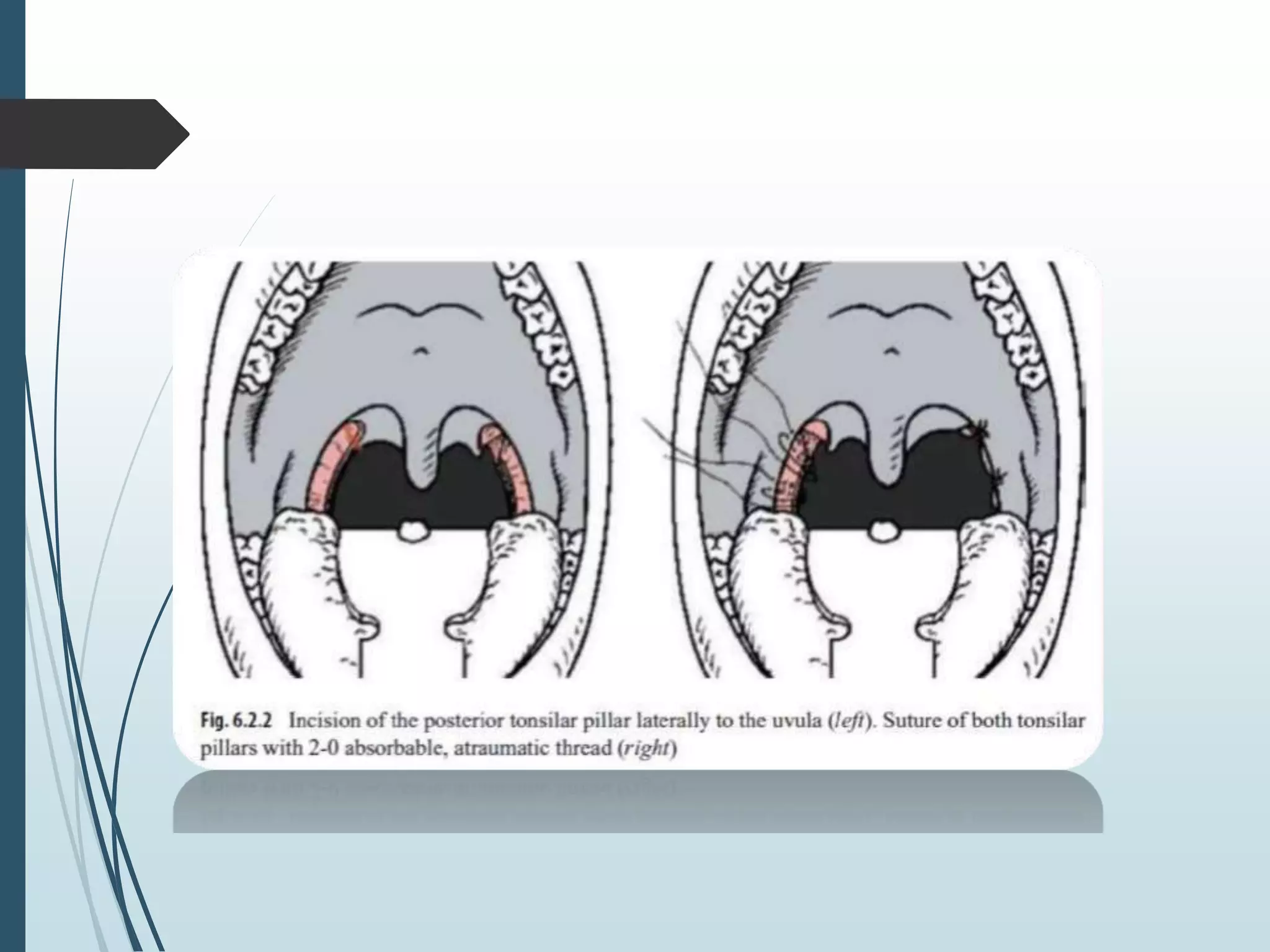
Obstructive sleep apnea (OSA) is a common chronic condition characterized by upper airway obstruction during sleep, leading to symptoms like snoring, daytime sleepiness, and potential cardiovascular issues. Diagnosis involves a detailed history and polysomnography, while management options include lifestyle changes, continuous positive airway pressure (CPAP), oral appliances, and various surgical procedures. Surgical interventions may be indicated in cases of severe OSA or when other treatments fail, offering significant symptom relief for affected patients.