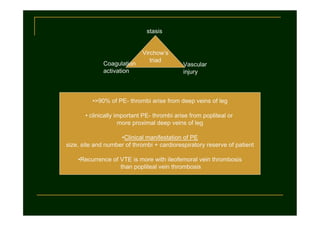
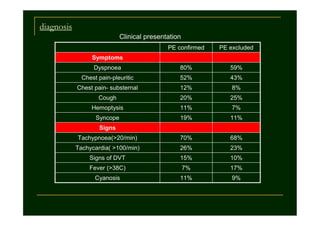
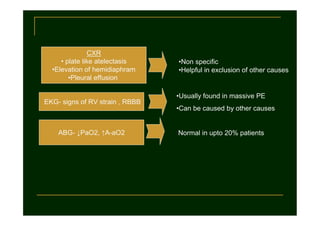
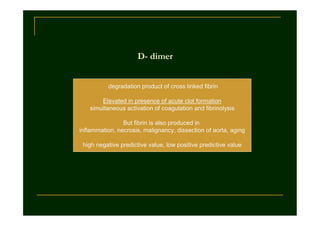
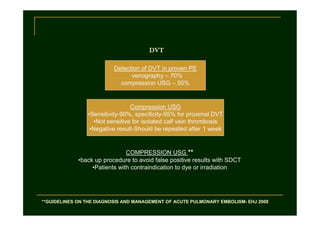
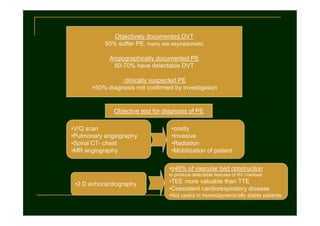
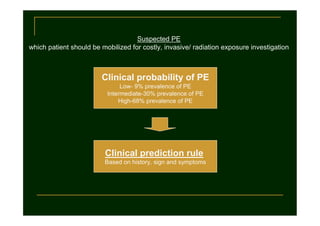
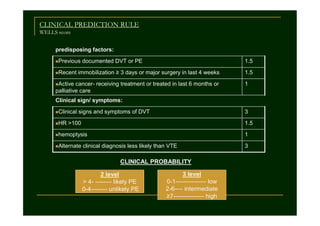
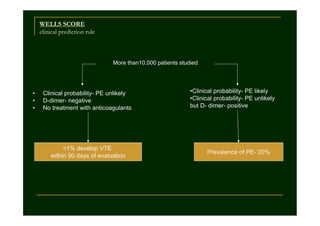
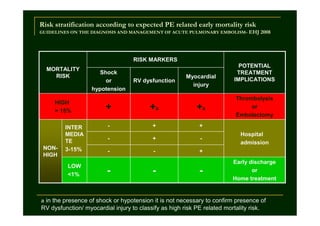
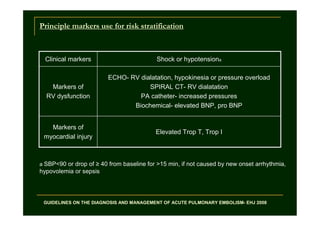
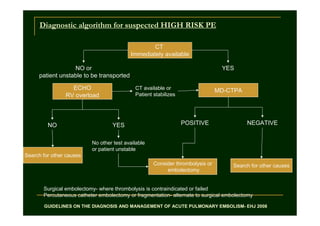
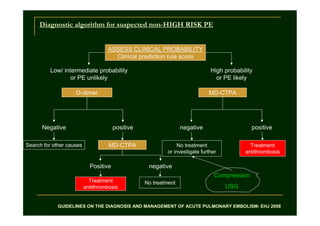
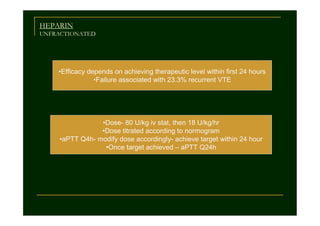
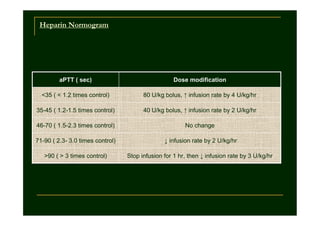
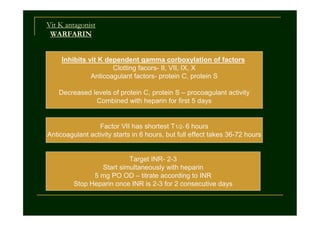
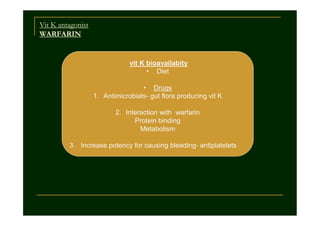
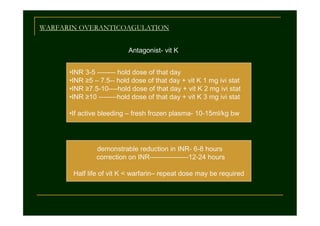
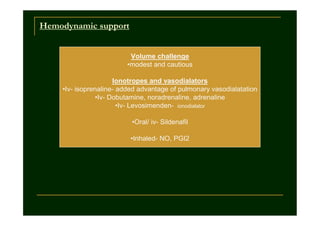
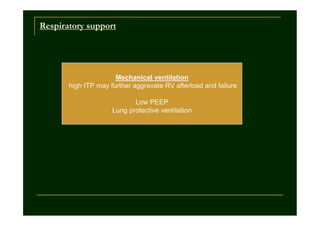
This document discusses venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE). It covers Virchow's triad as the underlying causes of VTE, clinical presentation of PE, diagnostic tests including D-dimer and imaging, risk stratification for PE-related mortality, anticoagulation treatment including heparin and warfarin, and hemodynamic and respiratory support for high-risk PE patients. Key points include that >90% of PEs originate from the leg deep veins, recurrence is higher for iliac vein thrombosis, and diagnostic algorithms involve assessing clinical probability and using tests like CT, ultrasound, and D-dimer.