The document provides information on recurrent patellar dislocation, including:
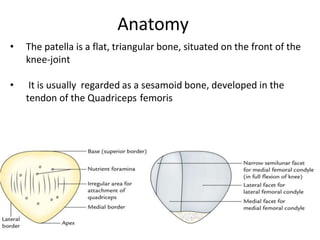
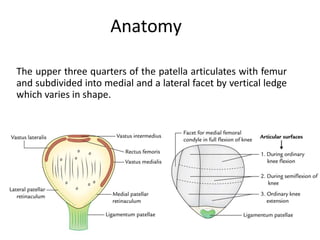
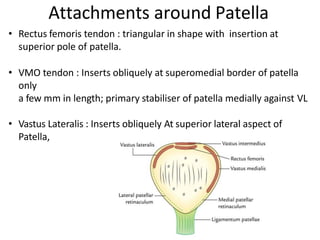
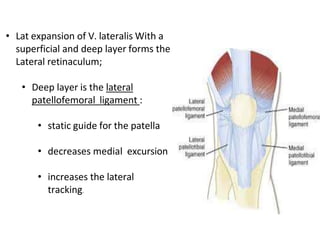
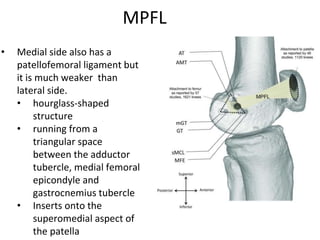
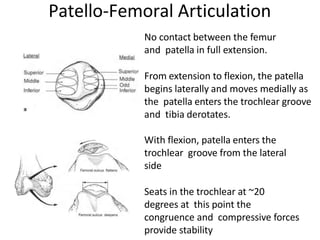
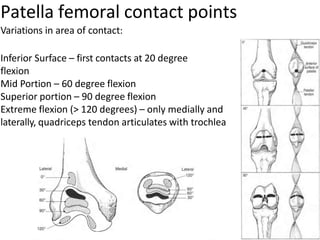
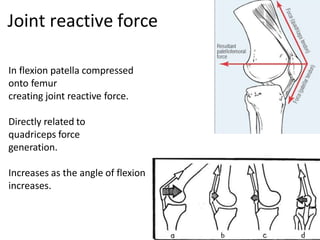
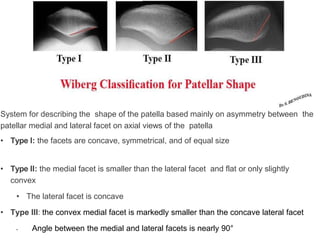
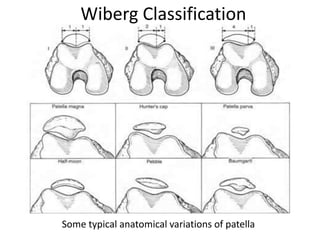
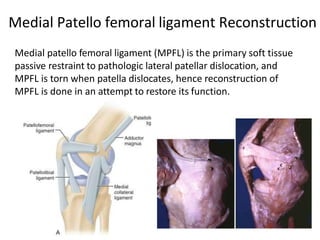
- Anatomy of the patella and its attachments
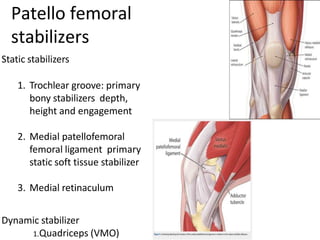
- Static and dynamic stabilizers of the patella
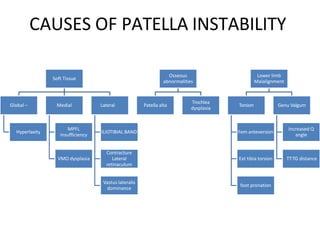
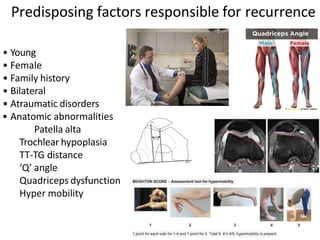
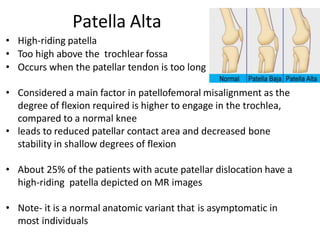
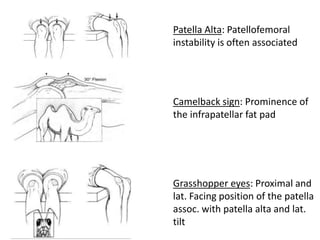
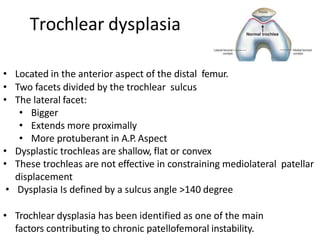
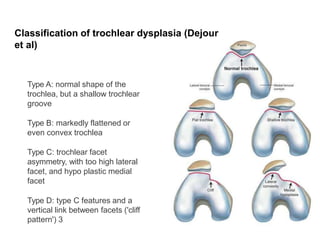
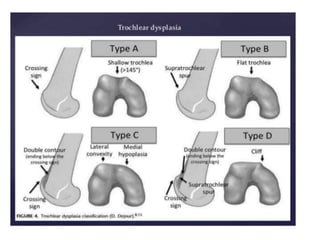
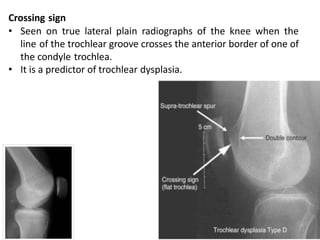
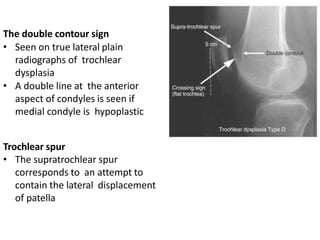
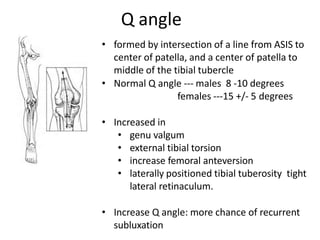
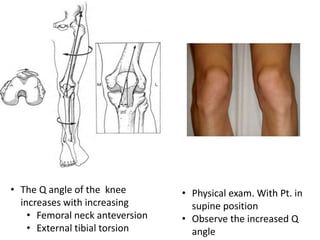
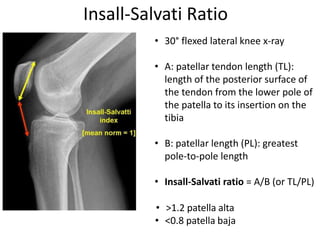
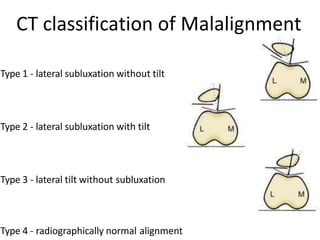
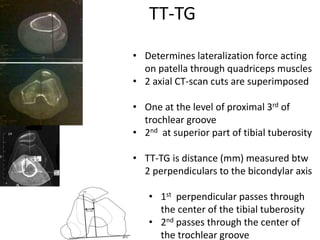
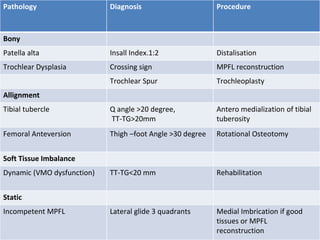
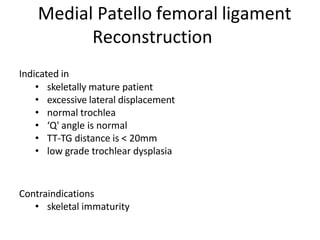
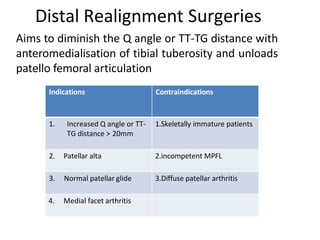
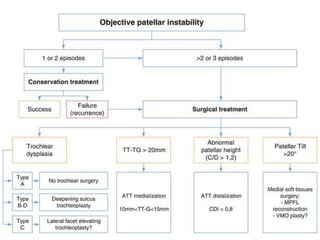
- Causes of patellar instability such as trochlear dysplasia, patella alta, increased Q angle
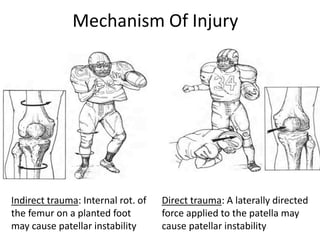
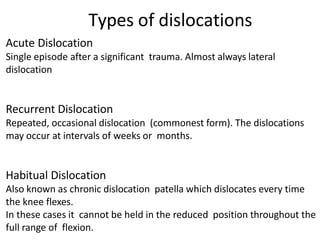
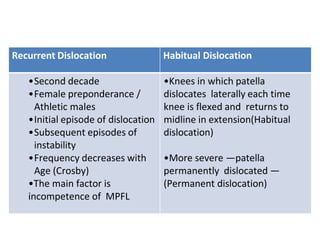
- Mechanisms of injury for acute vs recurrent dislocations
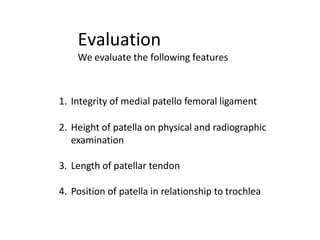
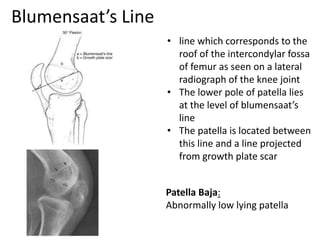
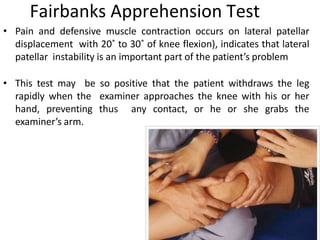
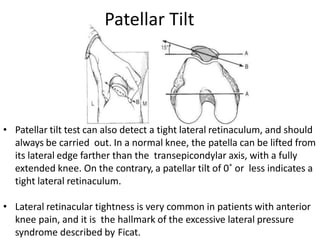
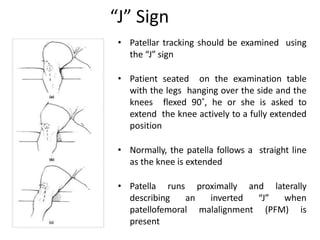
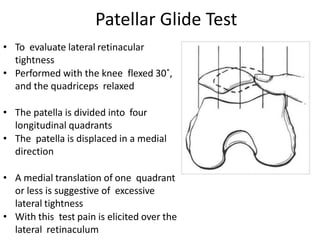
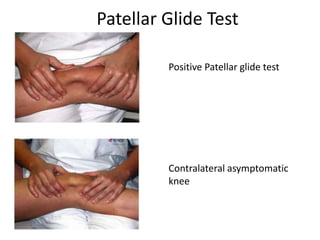
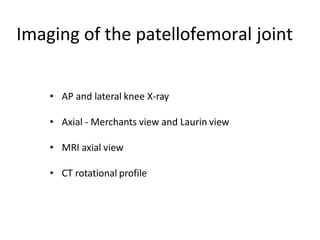
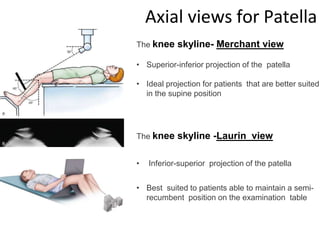
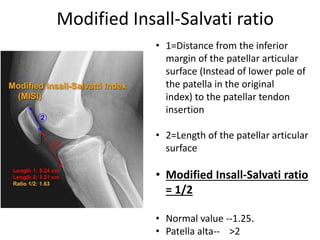
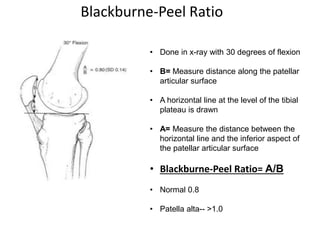
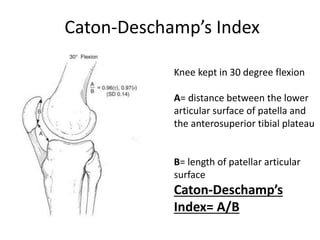
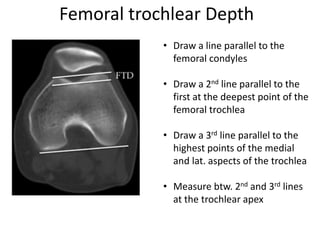
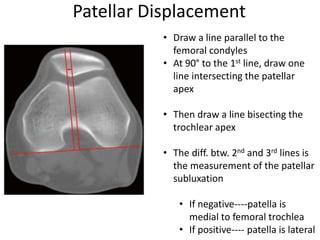
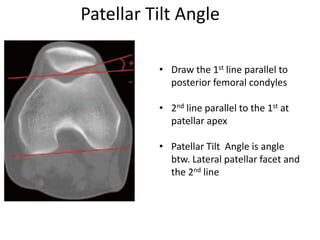
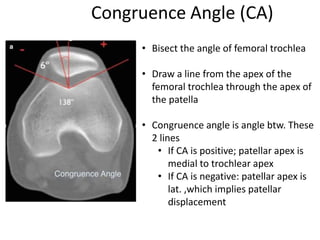
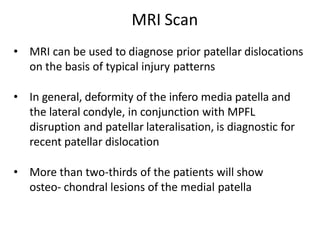
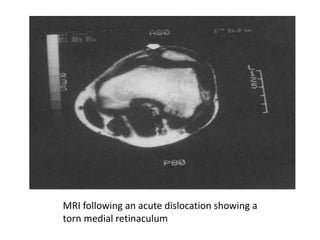
- Evaluation methods like the apprehension test, patellar glide test, and imaging views