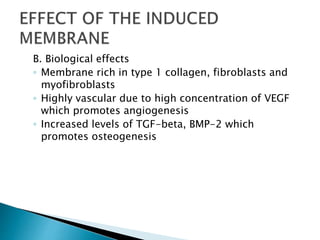
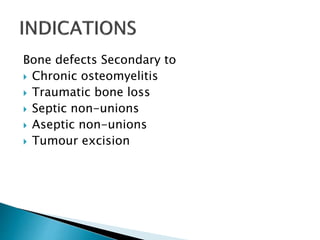
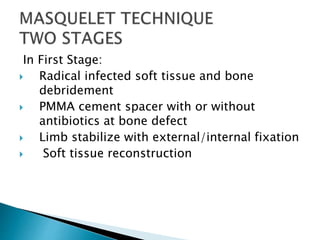
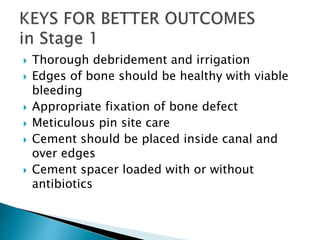
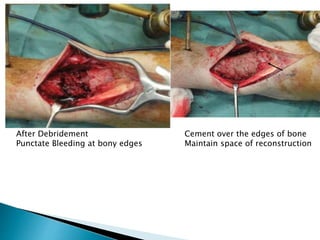
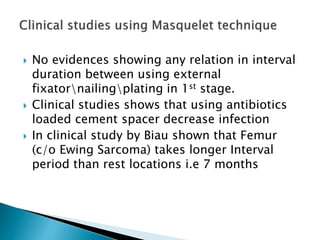
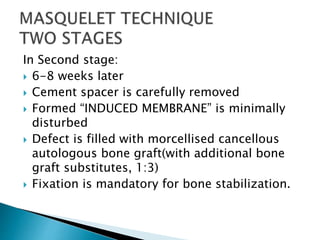
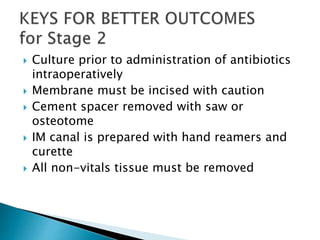
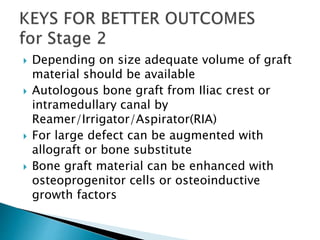
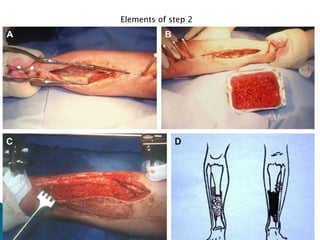
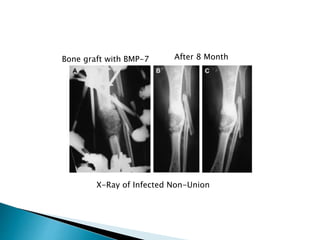
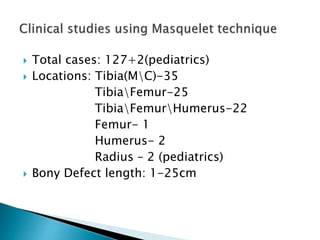
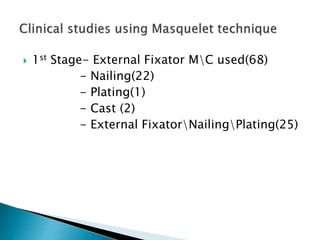
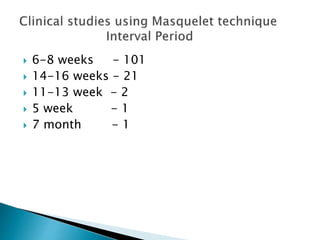
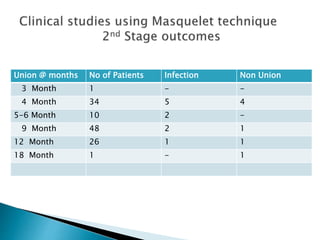
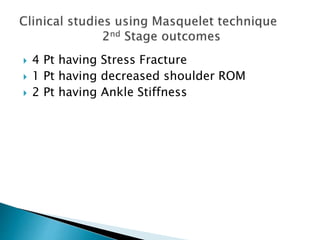
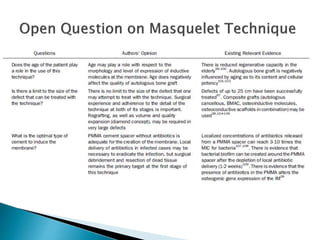
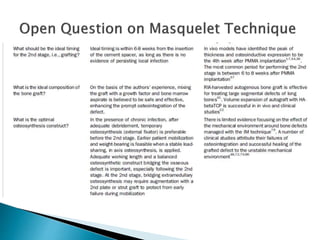
The document discusses the Masquelet technique, a two-stage procedure for treating bone defects and non-unions. In the first stage, radical debridement is performed followed by placement of an antibiotic-loaded cement spacer to form an induced membrane. In the second stage 6-8 weeks later, the membrane is preserved while removing the spacer and filling the defect with bone graft for reconstruction. Studies reported successful outcomes using this technique for various bone defects up to 25cm in length. Key factors for success include thorough debridement, maintaining the induced membrane, adequate stabilization and soft tissue management.