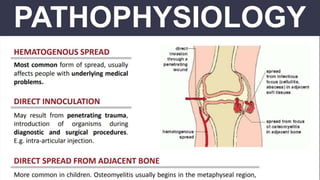
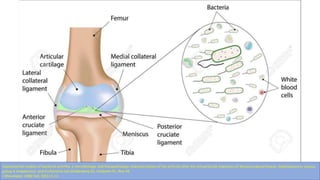
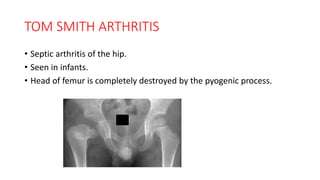
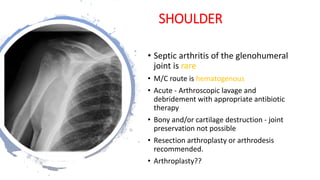
1) Septic arthritis is a orthopaedic emergency caused by bacterial or other infectious agents invading the joint space. Without prompt antibiotic treatment and drainage, it can cause permanent joint damage or systemic infection.
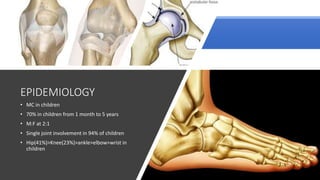
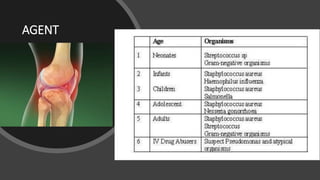
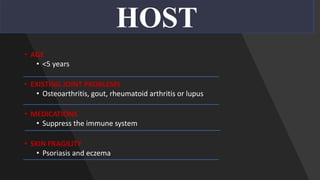
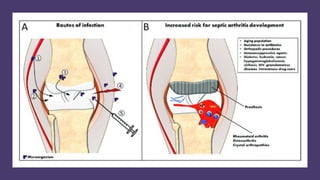
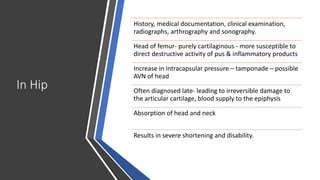
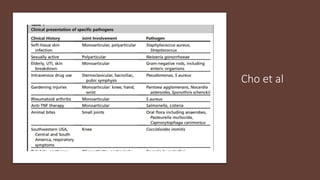
2) Risk factors include young age, existing joint problems, immunosuppression, skin conditions, and IV drug use. The knee and hip are most commonly affected.
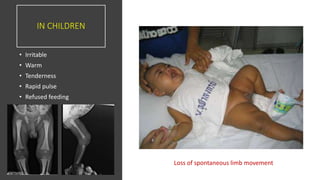
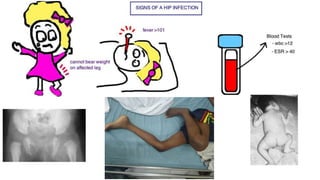
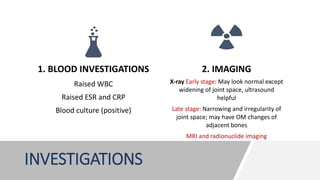
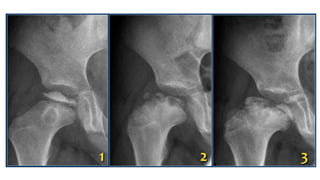
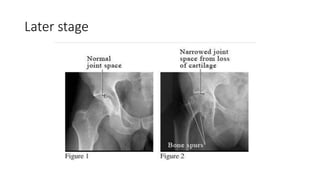
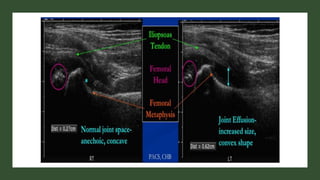
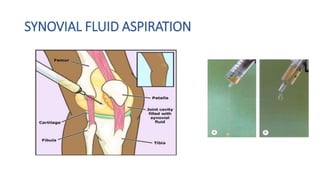
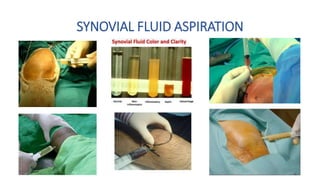
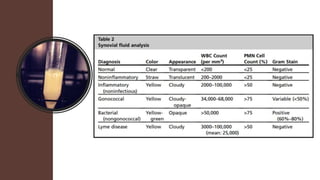
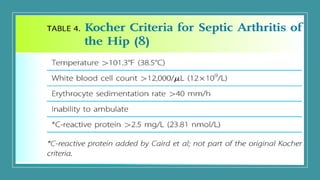
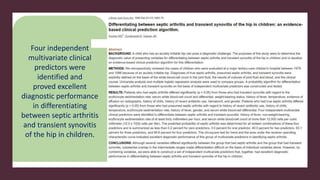
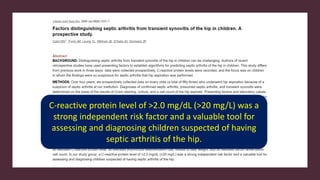
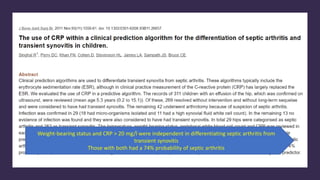
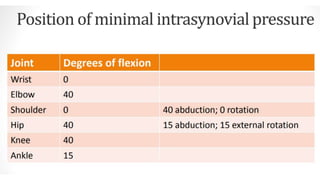
3) Clinical features include acute pain, swelling, warmth, and limited movement of the infected joint. Blood tests may show elevated inflammatory markers. Joint fluid analysis is required for diagnosis.
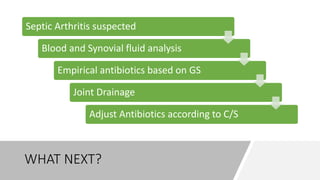
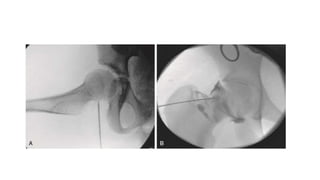
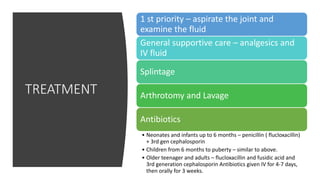
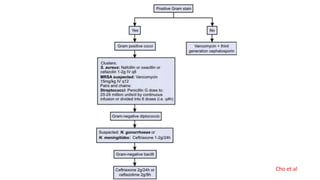
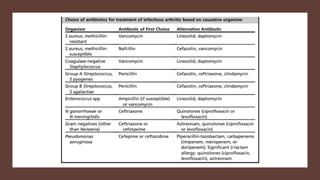
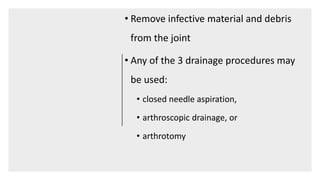
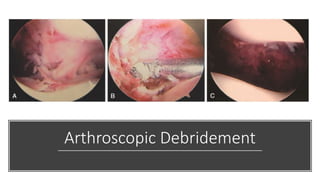
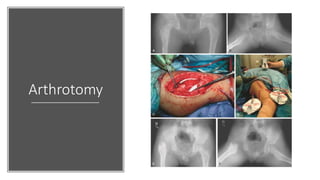
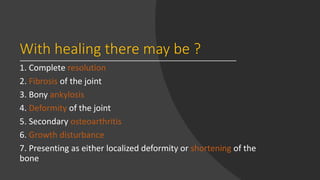
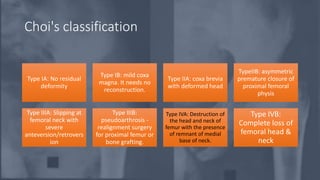
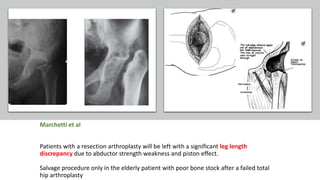
4) Treatment involves antibiotics, joint drainage, and sometimes surgery. Outcomes depend on early diagnosis and intervention, with possible sequelae including fibrosis, anky