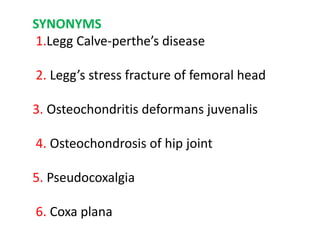
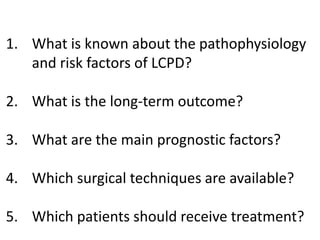
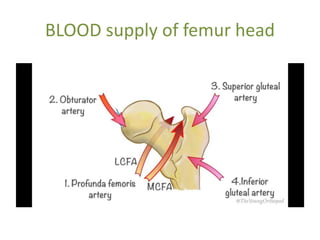
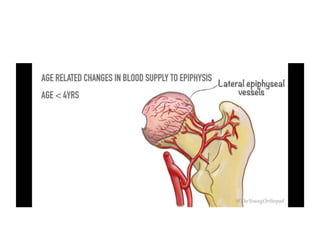
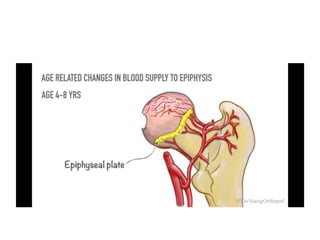
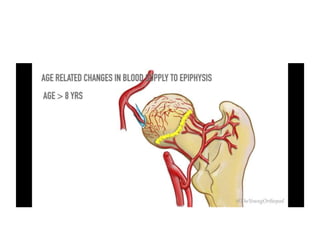
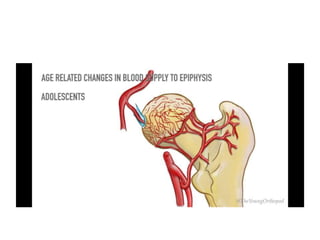
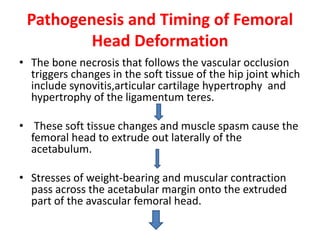
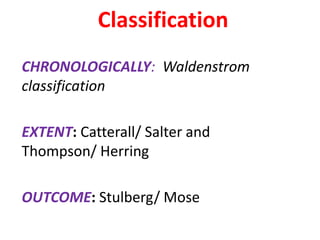
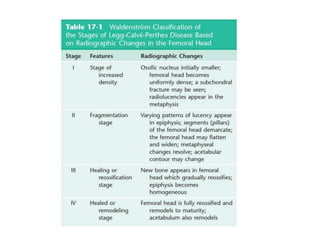
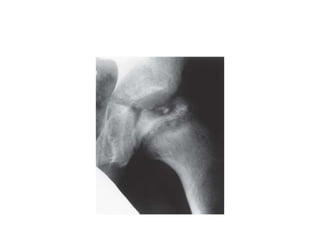
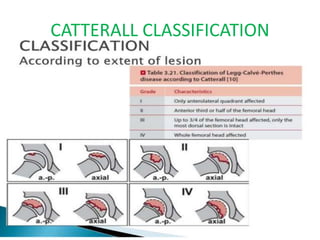
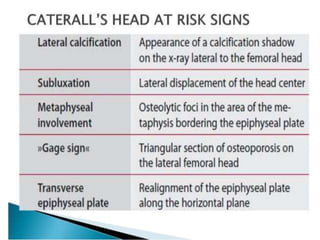
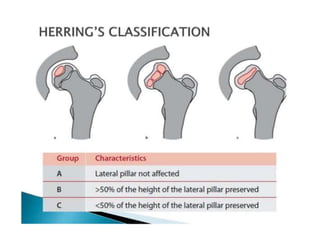
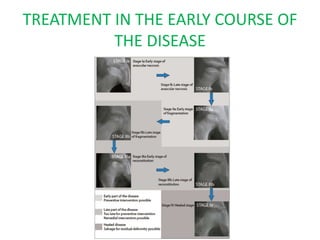
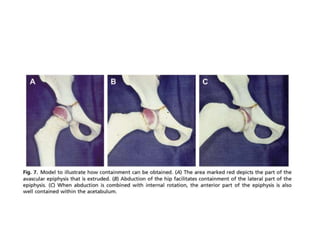
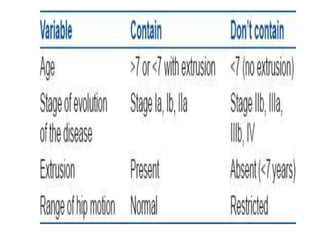
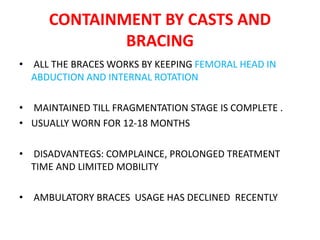
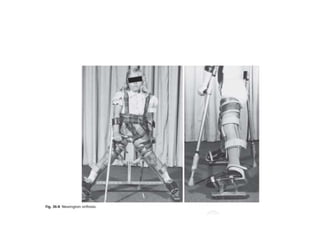
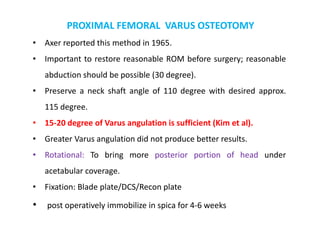
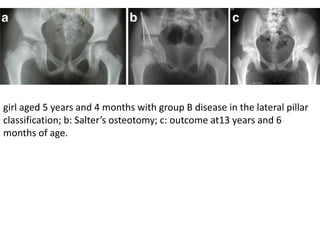
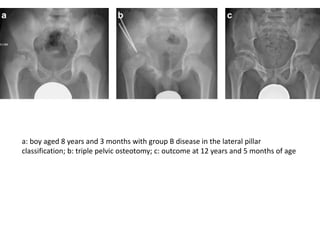
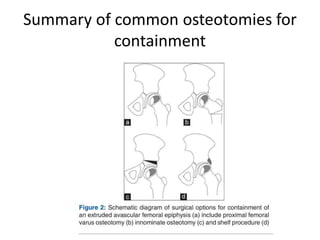
Legg-Calve-Perthes disease is a childhood condition caused by temporary loss of blood supply to the femoral head. It most commonly affects boys ages 4-8 and can cause deformity of the femoral head. Early containment of the femoral head via casts or surgery can prevent deformation and minimize long-term arthritis risk. Prognosis depends on the Herring classification, with surgery beneficial for lateral pillar group B/C cases after age 8. The goal of treatment is to maintain femoral head congruency and minimize secondary osteoarthritis.