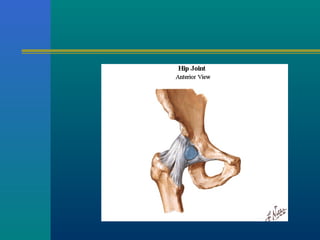
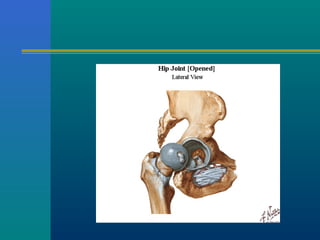
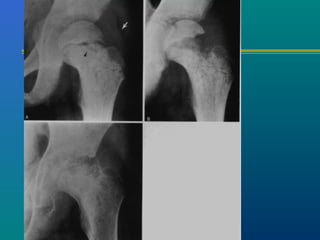
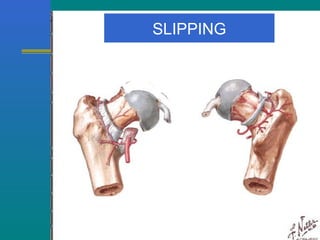
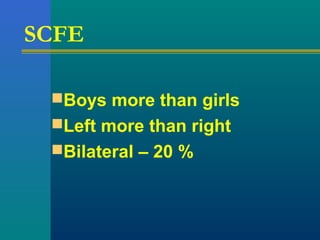
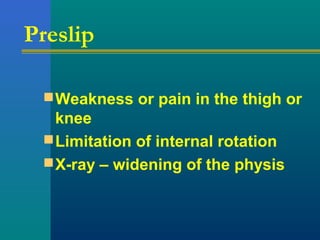
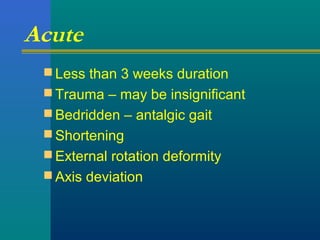
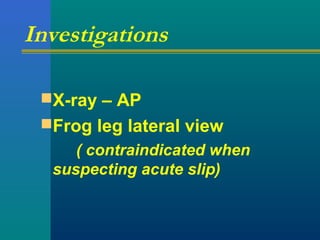
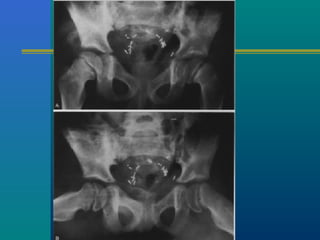
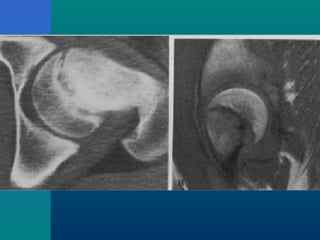
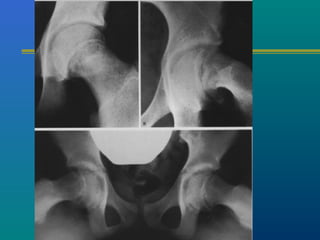
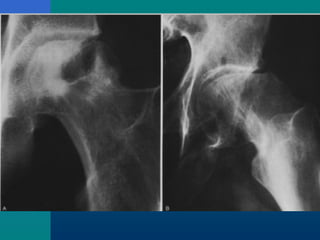
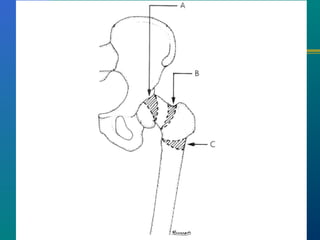
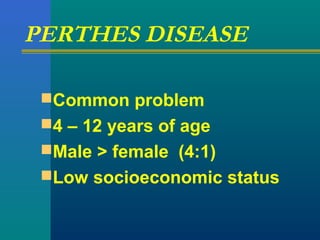
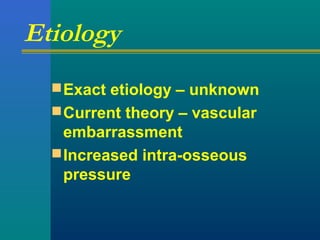
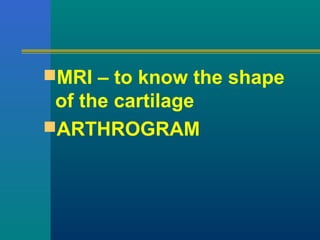
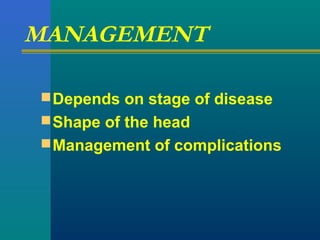
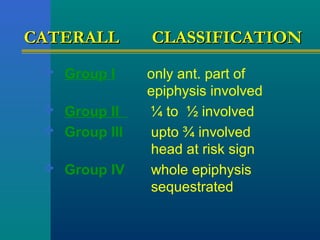
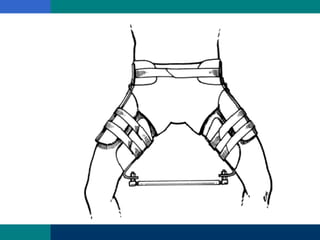
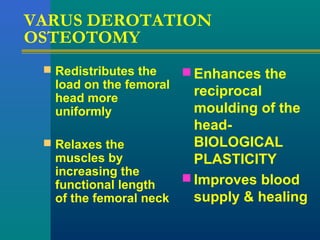
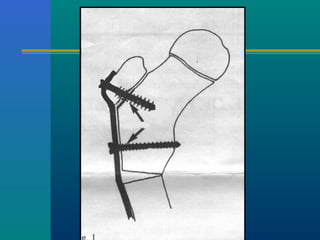
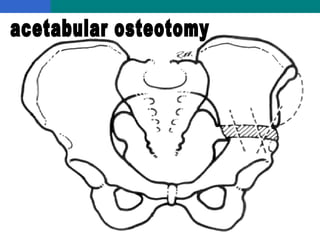
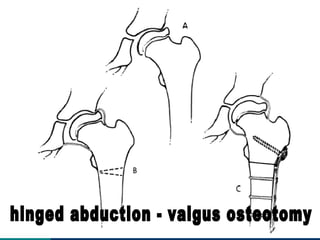
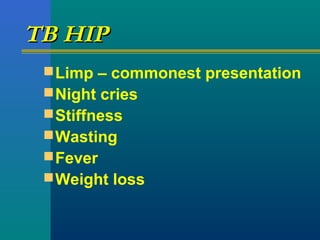
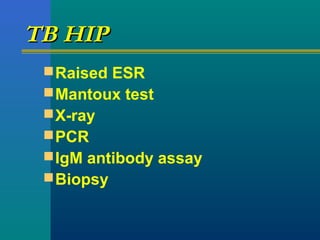
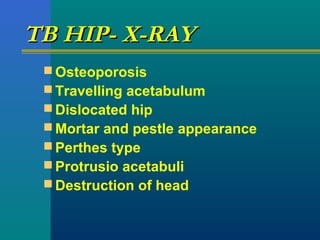
This document discusses several common causes of hip pain in adolescents, including transient synovitis, Perthes disease, slipped capital femoral epiphysis, septic arthritis, tuberculous arthritis, and idiopathic chondrolysis. For each condition, the document outlines typical presenting symptoms, potential causes, diagnostic methods like x-rays and blood tests, and treatment approaches such as rest, traction, surgery, or antibiotics. Common complications are also listed. The goal of treatment for many of these hip disorders is to relieve pain, prevent deformity, and restore hip function in adolescent patients.