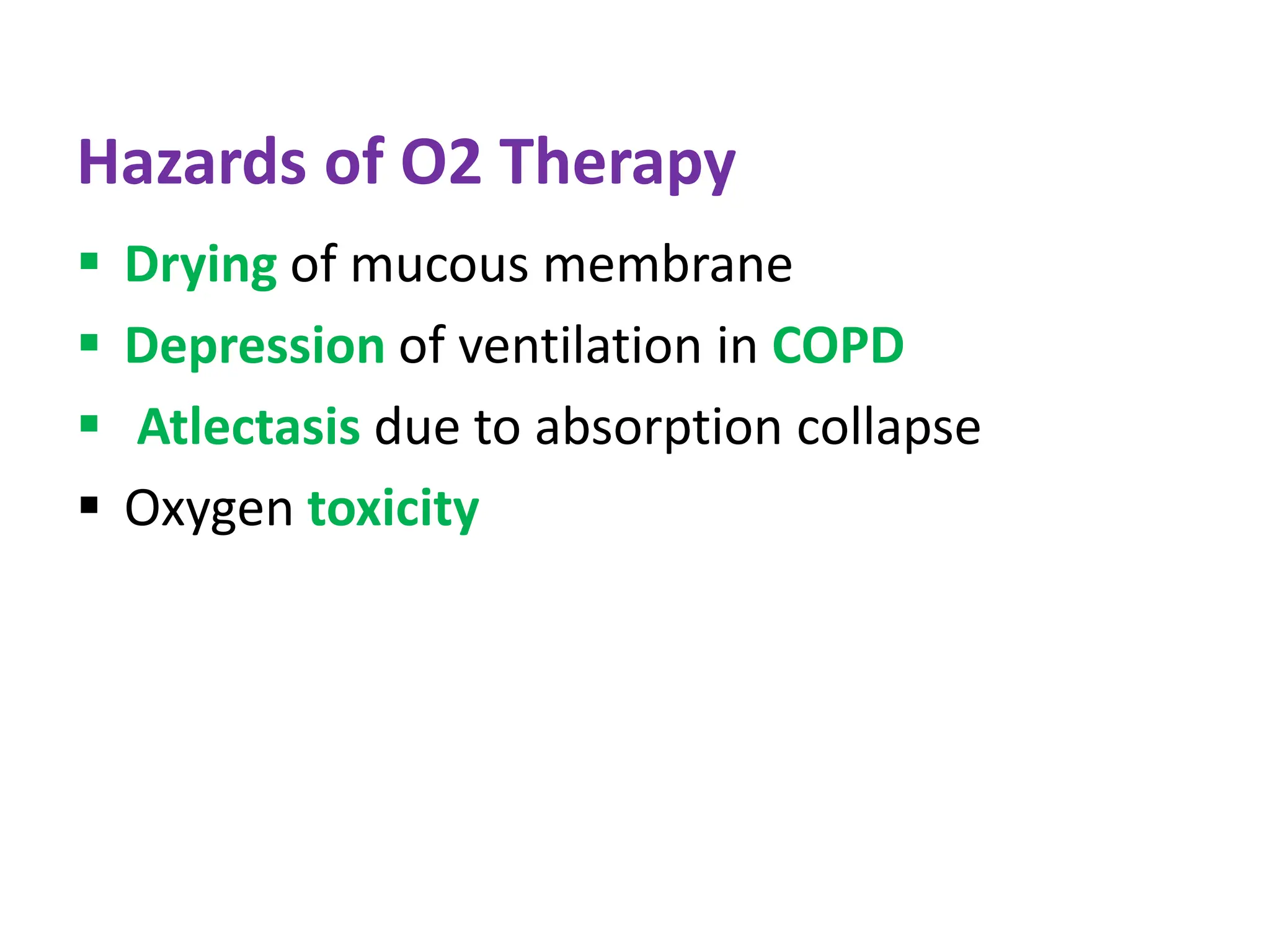
Oxygen therapy is used to treat conditions caused by low oxygen levels in the blood. It works by delivering oxygen through devices like nasal cannulas, masks, and ventilators at higher percentages than is found in regular air. The goals are to increase oxygen in the tissues and relieve symptoms. Different devices are used depending on the needed oxygen concentration and flow rate, ranging from low flow nasal cannulas for lower amounts to venturi masks or ventilators for higher amounts. Nurses must carefully monitor patients on oxygen therapy and watch for side effects like drying of tissues or oxygen toxicity from levels that are too high.