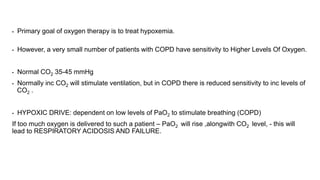
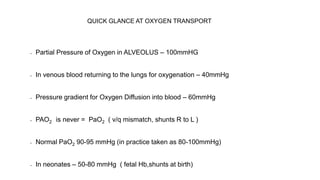
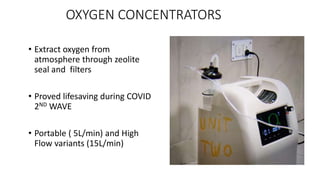
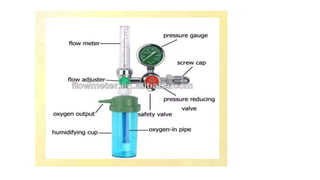
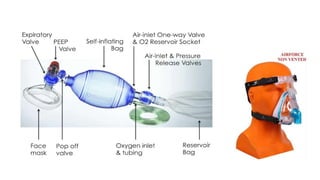
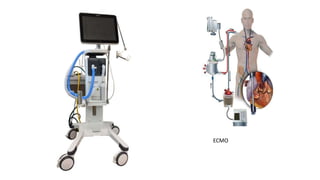
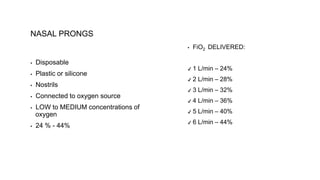
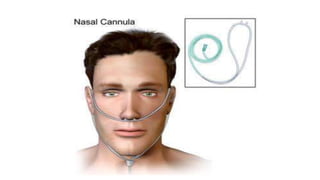
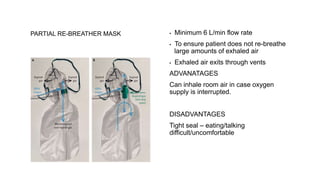
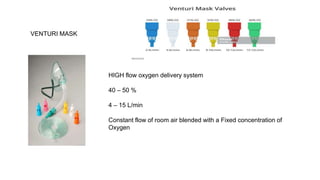
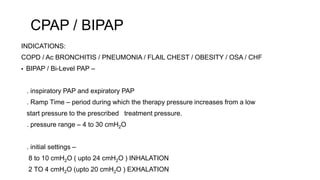
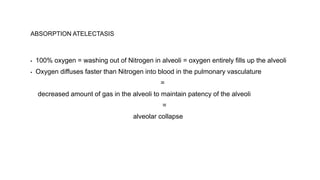
This document discusses oxygen therapy and its goals, methods of administration, and potential side effects. The primary goal of oxygen therapy is to treat hypoxemia by increasing oxygen delivery to tissues and preventing hypoxia. Various devices are used to administer oxygen at concentrations above 21% to meet patient needs, including nasal cannulas, masks, venturi masks, and CPAP/BiPAP. Potential side effects of prolonged high-concentration oxygen therapy include oxygen toxicity, retrolental fibroplasia, and absorption atelectasis. Careful titration of oxygen is required to maximize benefits and minimize risks.