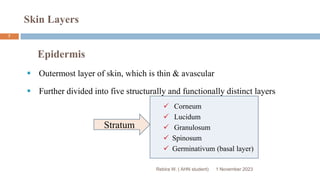
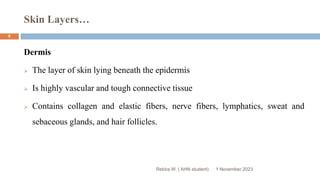
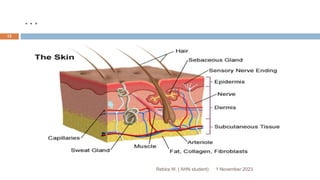
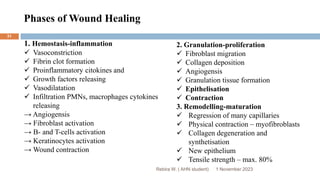
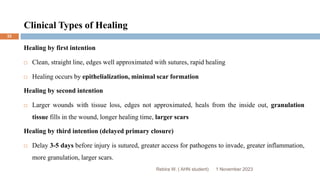
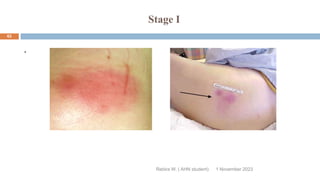
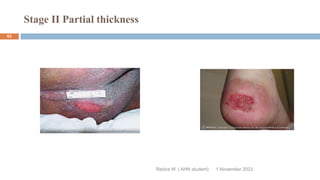
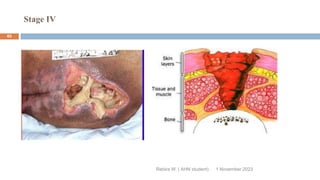
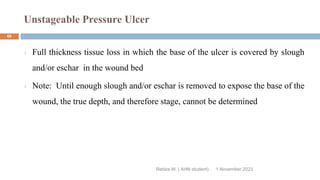
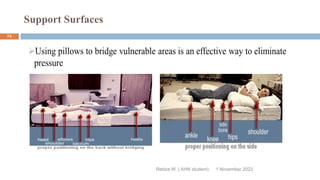
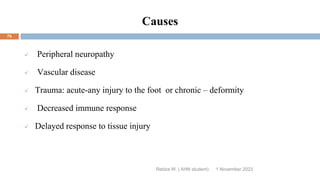
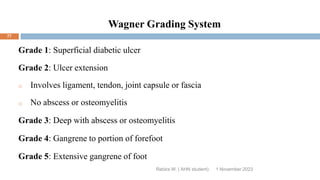
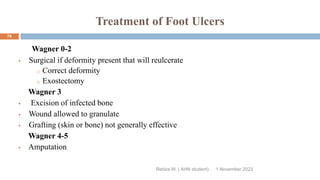
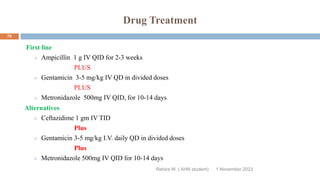
This document outlines a presentation on wound management given by Rebira W., a student in the Adult Health Nursing postgraduate program. The objectives of the presentation are to describe the structures and functions of skin, understand the impact of wounds on quality of life, identify different types of wounds and factors affecting wound healing, and know how to manage both acute and chronic wounds. The presentation covers topics such as the anatomy of skin and its layers, types of wounds classified by origin, the phases of wound healing, and managing specific wound types like pressure sores and diabetic foot ulcers.